46:1 ratio of car repair cost to failed part cost
Happy National Odometer Day to those who celebrate…
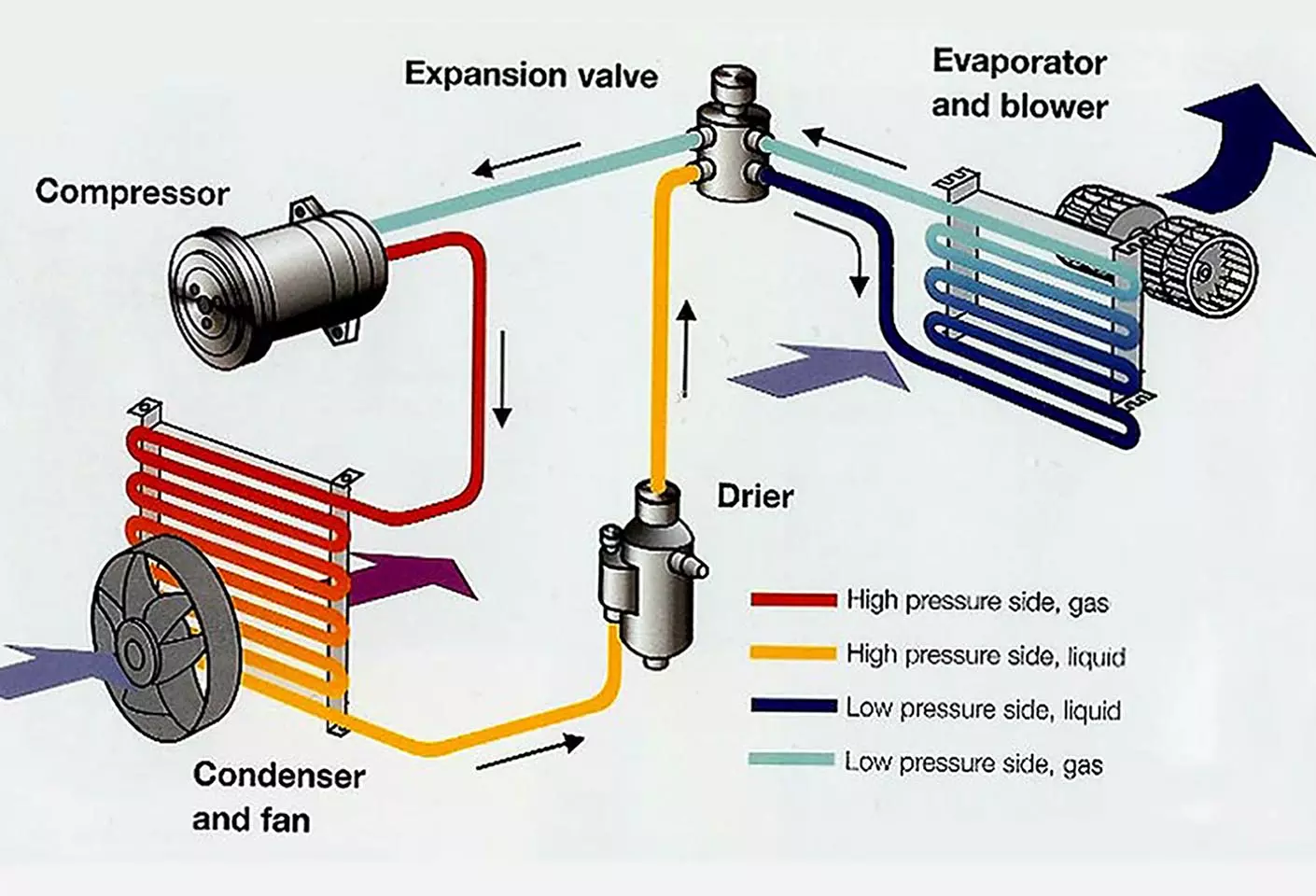
By taking a car to the dealer three times, I learned how white women with Long COVID feel. After every visit, the dealer said “Your AC is working perfectly.” On the fourth visit, the diagnosis was “There is no refrigerant in your system. It all leaked out from a failed receiver drier.” Because of Climate Change, I had no idea what a receiver drier was. From the Interweb:
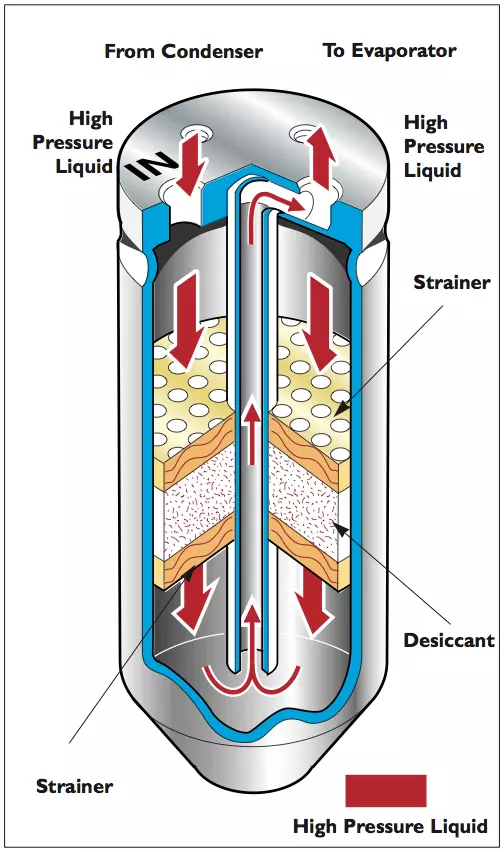
1.They act as a temporary storage container for oil and refrigerant when neither are needed for system operation (such as during periods of low cooling demand). This is the “receiver” function of the receiver drier.
2.Most receiver driers contain a filter that can trap debris that may be inside the A/C system.
3.Receiver driers contain a material called desiccant. The desiccant is used to absorb moisture that may have gotten inside the A/C system during manufacture, assembly, or service. Moisture can get into the A/C components from humidity in the air. This is the “drier” function of the receiver drier.
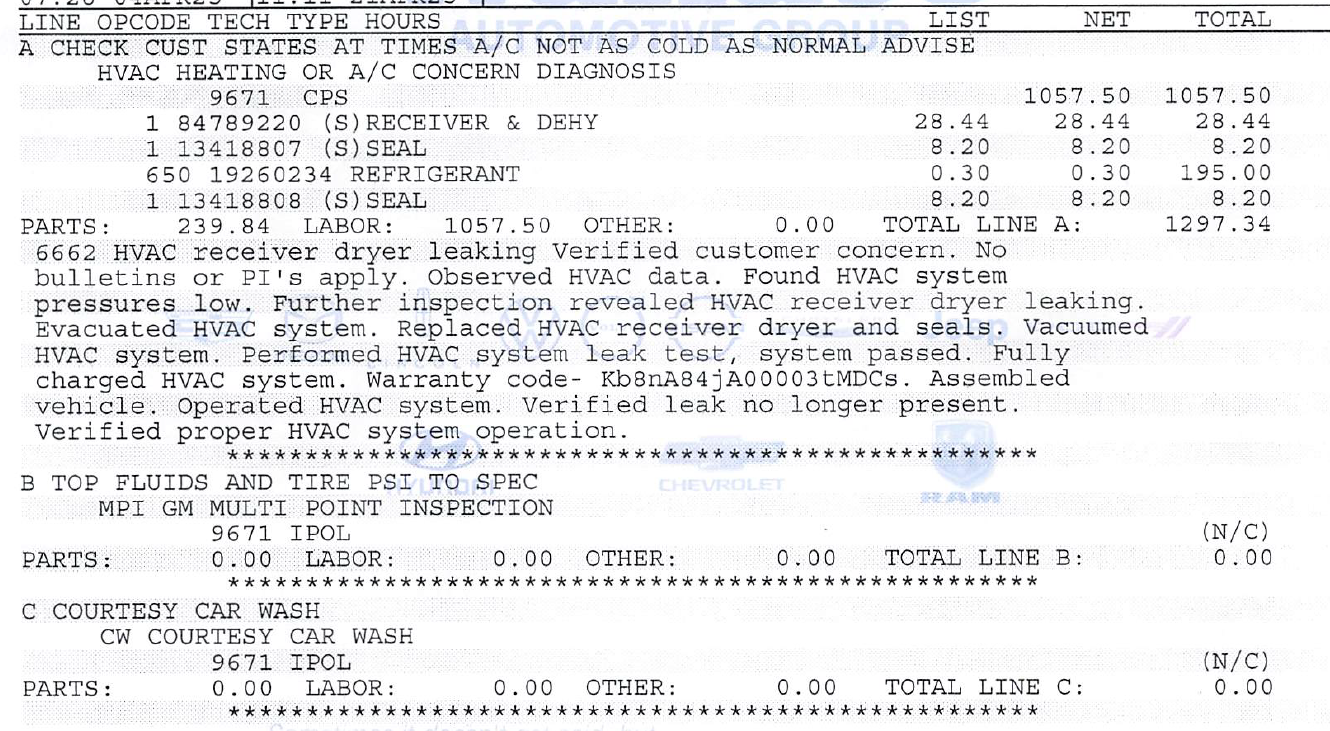
It turns out that this is a $28.44 authentic General Motors part, including dealer markup. The total repair bill was nearly 46X this amount, however, at $1,297.34. I have to believe that this is some kind of record.
(Fortunately, the entire cost was covered by a $2,600 GM Protection Plan that I had purchased after hearing frightening tales of $25,000+ transmission replacements. The 2022 Chevrolet has only about 7,000 miles on it and will be covered by this extended warranty until it is 11 years old.)
It is a little tough to understand how the labor added up to $1,057.50. The shop’s nominal rate is $225/hr so that would be 4.7 hours of labor happening between the 7:45 am dropoff and 10:53 am “your car is washed and ready” pickup. Perhaps, though, this also includes some diagnosis time from Service Visit #4? Friends who’ve been getting Toyota and Audi repairs in Maskachusetts and Florida have reported some huge labor estimates/charges relative to the flat rate labor hours found with a Google search and/or the actual time the car spent in the shop. Dealers seem to be quoting and getting fixed prices that work out to $300-400/hr. for their labor. I wonder if car care has become like human care: you’ll pay a way higher price if you don’t have insurance and, therefore, it makes sense to buy “insurance” even when you don’t need the insurance part of the insurance (i.e., to shift the risk). Or just buy a high-quality Georgia-built Kia with its 5-year bumper-to-bumper warranty and 10-year powertrain warranty (Kia achieves its superb quality without the benefit of union workers).
Separately, let’s raise a glass of DOT 3 brake fluid to our 2021 Honda Odyssey (built in Alabama by non-union workers who rejected a UAW organization effort). After 4.5 years and 50,000 miles it has suffered exactly 0 failures of any kind. (The only expenses have been for maintenance items, such as oil changes, wiper blades, battery, tires, and brakes.) Due to the miracle of Bidenflation, the minivan is currently selling, in nominal dollars, for almost exactly what we paid for it (survey of similar-mileage Odysseys offered by dealers).
Full post, including comments