I’ve now done enough coronary artery bypass graft (CABG) surgeries to learn the typical sequence:
- Surgeon arrives for “time out” (checklist review to prevent, e.g., wrong side operation), then leaves the room for the physician assistant to harvest the saphenous vein. The anesthesiologist performs a trans-esophageal echocardiogram to visualize pre-graft cardiac function.
- Surgeon reappears for scrub-in.
- I struggle to find space for myself between the perfusionist console and the surgical tech table while the surgeon and PA make the incision and perform the sternotomy.
- I watch from behind as the surgeon harvests the left internal mammary artery (“LIMA”, however the latest term: “left internal thoracic artery”)
- Surgeon has me switch with the physician assistant (PA). Surg tech hands me the cannulation equipment
- Surgeon tells me where to pick up the pericardium with the DeBakeys (non traumatizing forceps) to apply tension. The surgeon incises and throws sutures into the pericardium. We grab the sutures to fold back the each side of pericardium for better visualization of the beating heart.
- Cannulation time: the surgeon throws circular sutures (one or two, depending on preference) into the aorta and right atrial appendage. The heart is beating so the surgeon times the throws (needle push through tissue) based upon the relaxation of the heart. Once thrown, I grab each suture, cut the needle, and thread the suture through a rubber tube. I hand the surgeon the venous cannula, and he punctures the right atrium in the marked circle. I then pull the suture tight while pushing on the rubber tube. This tightens the suture around the cannula to create a seal. Repeat on the aorta. Every time I touch the heart, the screen shows an ectopic beat.
- We clear the air from the tubes and clamp the aorta proximal to the aorta cannulation site. The surgeon announces to the perfusionist to go “on pump”. The surgeon will tell the perfusionist to infuse cardioplegia (cold solution of high potassium) that paralyzes the heart. Blood pressure flatlines at around 90mm of mercury (as opposed to the usual rise and fall with the heartbeat).
- Anastomosis: The surgeon identifies areas to bypass the blockages. While he looks, I ask to make sure I know what vessel he is thinking about. “That’s the Left Anterior Descending artery?” He responds, “No, he has a small LAD, this is actually the OM1.” The surgeon and PA wear loupes to see the 6-0 suture (0.33mm diameter) to bring the vessels together. First is the graft-coronary anastomosis, then the aorta-graft anastomosis. The PA “follows” the surgeon’s throws to prevent “locking” the suture. I use the “blower” to blow a thin stream of air into the field to provide better visualization of the vessels (one attending barks at me: “it takes forever to de-air the left ventricle”). I am also in charge of squirting water onto the surgeon’s hands while he or she ties the suture. Each anastomosis takes about 10 minutes and is done in a quiet OR.
- Anastomosis is complete. Surgeon uses a doppler to confirm patency and good flow.
- Anesthesiologist reports on cardiac function. Frequently, there will be immediate improvements in the regions that were impaired.
- Surgeon inserts ventricle and atrial pacer wires and pushes them out through the skin.
- Surgeon inserts drains (“chest tubes”) into the pericardial and pleural spaces. The nurse connects them to suction.
- Perfusionist stops cardioplegia, and warms the blood. The heart begins to beat slowly, then goes into ventricular fibrillation. The surgeon takes the paddles and defibrillate the heart into sinus rhythm.
- Surgeon closes the sternum with stainless steel wire and scrubs out.
- Time to close. Usually I work with the 45-year-old head surgical PA, who patiently tries to teach me all of her chest-closing tricks. “We close differently than downstairs [in general surgery]. In the thorax, no space is allowed or it could blow up into a raging infection.” She instructs me, “Take smaller bites.” We close in multiple layers, typically 3-4 to ensure there is no potential space for fluid to accumulate. After the second operation, I am able to close three inches of the 10-inch incision before the PA meets me in the middle. “Good job, you are teachable.” (on the first two, she redid my sutures because they were too far apart)
Medical students are required to skip cases on Thursday to attend a Dean’s session highlighting a “medical topic of critical importance,” one of three each year. The topic this week is “LGBTQ myths and medical miracles” and the speaker (“Dr. Castro”) is an internist from San Francisco. “How many of you have heard of Stonewall Inn? This is recognized as kicking off the Gay Pride and fighting for gay rights. I went to medical school in the 1980s. We had a psych lecture titled, ‘Homosexuals, pedophiles, and beastiality.’ I give this timeline to highlight the challenges people have overcome, and the amazing change in perspective in such a short amount of time. I want to remind everyone that this fight is still ongoing. Look at Pulse Nightclub, an evil that should shake every American. Look at Trump trying to say sex is not gender identity, and that anti-discrimination laws do not apply to us.”
[Editor: Why would LGBTQIA+ community members want anti-discrimination laws to apply to them? Generally these laws cover classes of workers whom employers regard as inferior, e.g., older or disabled workers, racial groups with low academic achievement, etc. Would it help gay physicians, for example, if the government officially says “Because of their evening sexual activities, these doctors will not be able to treat patients as well and therefore you shouldn’t hire them unless you’re forced to”?]
He pauses. “How many of you are in a target group?” Half of the hands go up. Dr. Castro: “Every single one of you should raise your arm. Every woman should raise your hand, you don’t get equal pay for equal work. If you have any degree of pigmentation in your skin, raise your hand; you are a victim.”
The first slide contains only the text, “If we can get to sensitive.” Dr. Castro asks the class, “Let’s say a close friend came out as gay. How would you feel?” The first answer, “I would not care,” turns out to be wrong. “Embarrassed he did not tell me sooner,” and “Proud they trusted me” were received with approval.
Nobody was willing to go on record with an anti-gay sentiment, so the speaker had to step in and play the role of the prejudiced. His stereotypical anti-gay sentiments included “They walk around in Speedos at Pride festivals,” and “Are children raised by gay couples at a disadvantage?”
[Editor: “Growing up with gay parents: What is the big deal?” (Linacre Quarterly 2015, a bioethics journals) reviews the research on the last topic. Sample:
A 2013 Canadian study (Allen 2013), which analyzed data from a very large population-based sample, revealed that the children of gay and lesbian couples are only about 65 percent as likely to have graduated from high school as are the children of married, opposite-sex couples. The girls are more apt to struggle academically than the boys. Daughters of lesbian “parents” displayed dramatically lower graduation rates. Three key findings stood out in this study: children of married, opposite-sex parents have a high graduation rate compared to the others; children of lesbian families have a very low graduation rate compared to the others; and children in the other four types of living arrangements (common law marriage, gay couple, single mother, and single father) are similar to each other and fall between the extremes of married heterosexual parents and lesbian couples.
]
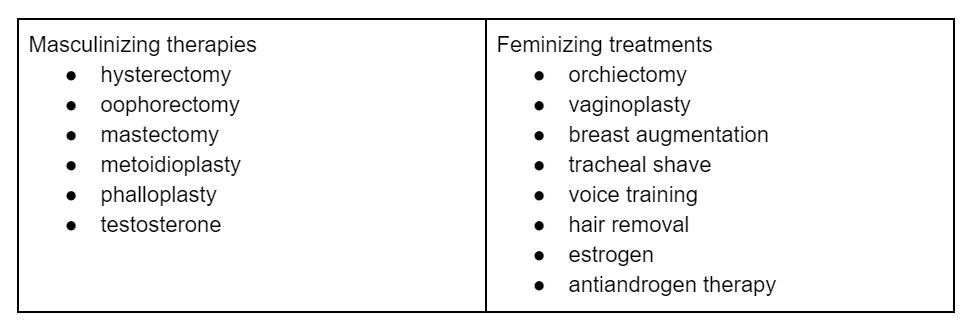
Dr. Castro explains, “One of the critiques from last year’s session was that there wasn’t enough medicine in this talk. So let’s talk about some of the medical treatments available for gender dysphoria.” Slide with two columns:
Gigolo Georgio asks, “Does insurance cover these treatments?” Dr. Castro: “Right now typically not, but we can get around this sometimes by using a different diagnosis. For example, a patient may have a fibroid that wouldn’t typically be an indication for a hysterectomy, but under this situation it can be. Or if the patient has a questionable breast mass, we decide that it should be removed.” The big event recently is we now have a DSM code for gender dysphoria. If we as advocates continue to persist, insurance companies will eventually pay for treatments with this DSM code.”
[Editor: “Long-Term Follow-Up of Transsexual Persons Undergoing Sex Reassignment Surgery: Cohort Study in Sweden” (2011): “Persons with transsexualism, after sex reassignment, have considerably higher risks for mortality, suicidal behaviour, and psychiatric morbidity than the general population. Our findings suggest that sex reassignment, although alleviating gender dysphoria, may not suffice as treatment for transsexualism, and should inspire improved psychiatric and somatic care after sex reassignment for this patient group.”]
Dr. Castro talks about the challenges faced by his transgender patients: “My patients usually shy away from the spotlight. They work night jobs, or at a call center. Several are truck drivers. All transgenders are marginalized early which leads to distrust in systems, including the medical system. Many were kicked out by their family, had trouble finding a job, many drop out of school due to bullying. One in four attempt suicide by 25. One in five who come out are kicked out by their PCP. There is no way to reverse this overnight.” Type-A Anita is the first to respond. “How do we fix this?” Dr. Castro: “It will take concerted effort. For example, educating medical staff on proper pronouns, and redesigning medical forms and EMRs into gender neutral forms.”
Statistics for the week… Study: 6 hours. Sleep: 7 hours/night; Fun: 1 night. Example fun. Jane, Luke, Samantha, and I grab beers and burgers. Samantha gets $5,000 per year for CME at her HCA hospital job. She and a colleague (also a PA) just returned from a hospitalist conference in Oregon.
Over dinner, we discuss media coverage of hospitals taking poor patients to court and garnishing wages. A large academic center (University of Virginia) was featured for pursuing patients whereas the for-profit HCA hospital was more charitable. Samantha: “HCA doesn’t divert. We will accept any patient even if our hospital is full. It is so bad right now that each hospitalist has 27-30 patients.” Jane, “I can’t even keep my 2-3 patients straight.” Jane continues, “The ED is full, we have patients being admitted, treated, and discharged all in an ED bed. It got so bad once that we converted the cath lab into beds. I have 17 patients. The hospitalists who are in charge and technically sign orders and notes for billing don’t ever see my patients.”
The rest of the book: http://fifthchance.com/MedicalSchool2020
“I can’t even keep my 2-3 patients straight.”
The coddling of the American medical student.