Loss of Rob Holland and David Paton, founder of Orbis
It’s World Pilot’s Day today, but I’m not celebrating. Rob Holland, whom the legendary Mike Goulian brought to my old home airport, died two days ago in an MXS-RH while preparing for an air show. Confusingly, Rob wasn’t doing any crazy-looking maneuvers just before the crash, but only returning for a normal landing. An aviation friend: “heard the engine broke off and took out Rob’s wing. The composite firewall breaking is a known issue with the MX airplane.” Here’s Rob with an air show spectator:
The first time that I went upside down in an airplane it was with Rob, instructing out of KBED in the Decathlon at the time. I saw him only at air shows after he escaped to tax-free New Hampshire, but I remember him as patient and unfazed by student incompetence. A great ambassador for aviation.
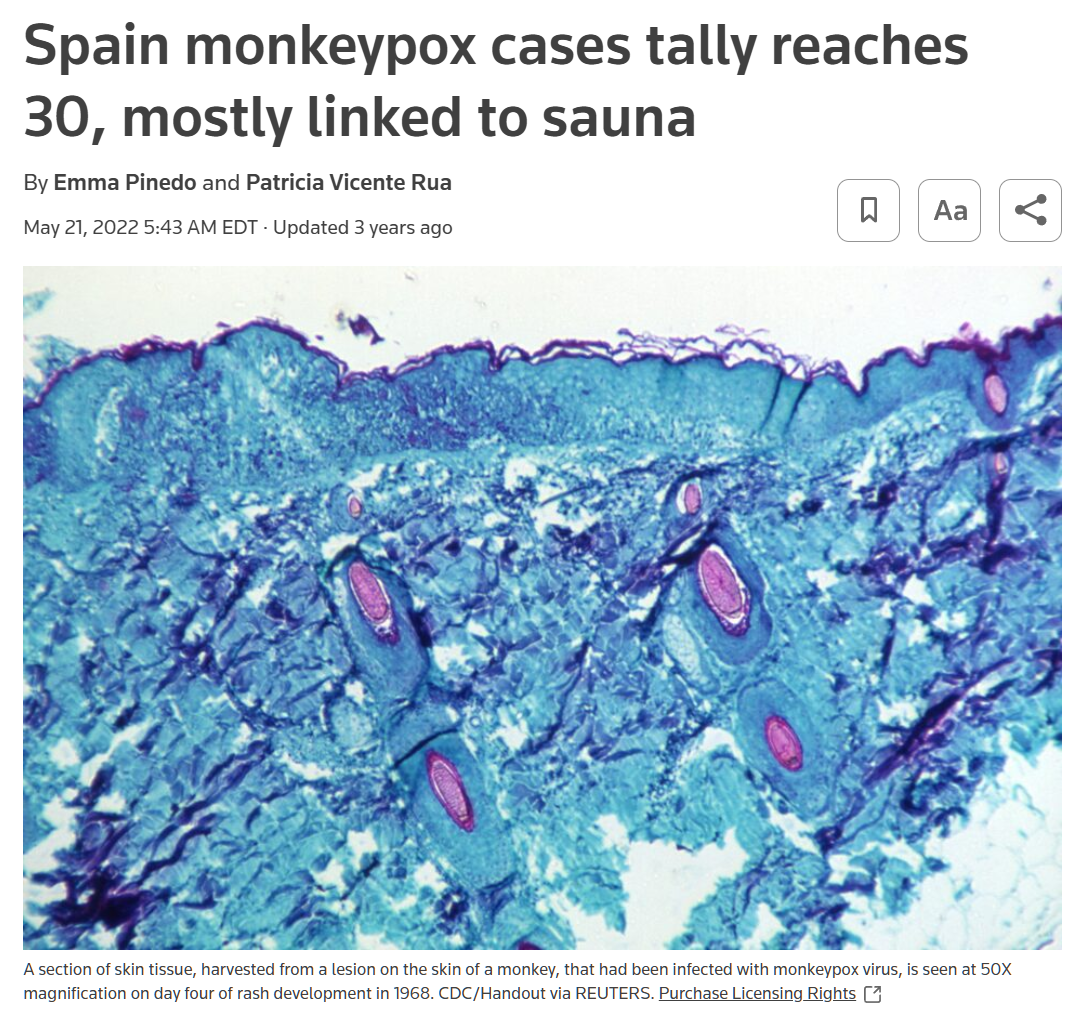
Also notable, though not a tragedy, David Paton, the 94-year-old founder of the Orbis flying eye hospital charity, has died. From the New York Times obituary:
David Paton, an idealistic and innovative ophthalmologist who converted a United Airlines jet into a flying hospital that took surgeons to developing countries to operate on patients and educate local doctors, died on April 3 at his home in Reno, Nev. He was 94.
The son of a prominent New York eye surgeon whose patients included the shah of Iran and the financier J. Pierpont Morgan’s horse, Dr. Paton (pronounced PAY-ton) was teaching at the Wilmer Eye Institute at Johns Hopkins University in the early 1970s when he became discouraged by increasing cases of preventable blindness in far-flung places.
(i.e., his life was consistent with the data presented in The Son Also Rises: economics history with everyday applications)
Before it decided to concentrate on Rainbow Flagism and Critical Race Theory, USAID pitched in to help spread ophthalmology knowledge to poor countries:
Dr. Paton decided to raise funds on his own. In 1973, he founded Project Orbis with a group of wealthy, well-connected society figures like the Texas oilman Leonard F. McCollum and Betsy Trippe Wainwright, the daughter of the Pan American World Airways founder Juan Trippe.
In 1980, Mr. Trippe helped persuade Edward Carlson, the chief executive of United Airlines, to donate a DC-8 jet. The United States Agency for International Development contributed $1.25 million to convert the plane into a hospital with an operating room, a recovery area and a classroom equipped with televisions, so local medical workers could watch surgeries.
(I’m not sure that $1.25 million would pay for new carpet and a coffee maker in a Gulfstream today.)
David Paton wasn’t a pilot, but he created one of the greatest demonstrations of the power and value of aviation.
Some photos of the Orbis MD-10 at Oshkosh (EAA AirVenture) in 2021 (note the COVID-era mask, one of the few at Oshkosh that year):



Separately, if you need some help with your eyes in order to keep flying safely, U.S. News says to pack a bathing suit and go to Miami (ranked #1). Alternatively, pack a gun and ammo and go to Philadelphia (#2) or Baltimore (#3):
Circling back to Rob Holland, I think that he was truly one of those people whose personality in life matched his eulogy personality. Despite being a fierce competitor and top achiever, he never exhibited a touch of “pilot ego.” I will miss him.
Full post, including comments