AI goes to the bathhouse
An elite Californian posted with satisfaction a state-sponsored NPR story about how stupid people in Louisiana were, especially with respect to the mpox vaccine. I decided to see if ChatGPT had advice regarding avoiding mpox (not to be conflated with the racist “monkeypox virus”, which is the cause).
Prompt 1: Is there any lifestyle change that I could adopt to minimize my risk of catching mpox?
ChatGPT gives a one-page answer and the only reference to sex is “Use condoms and consider other barrier methods during sexual activity”.
Prompt 2: You mention “sexual activity”. Is there any particular kind of sexual activity that is more likely to result in contracting mpox?
ChatGPT gives a one-page answer that doesn’t hint at the type of person or group that might be infected.
Prompt 3: You say “If you are in a community experiencing an mpox outbreak or belong to a group at higher risk”. What would be an example of a “group at higher risk”?
ChatGPT gives a 1.5-page answer, buried within which is the phrase “Men Who Have Sex with Men (MSM)”
Prompt 4: If a person is a man who has sex with men and wants to avoid mpox, should he stop having sex with men?
ChatGPT gives a 1.5-page answer that can be summarized as “no”, but does note that “Reducing the number of sexual partners can lower the risk of exposure.”
Prompt 5: Would it make sense for public health officials to ban group sex activities by men who have sex with men in order to minimize mpox spread?
ChatGPT responds that this would not be “ethical” (but it is ethical to close schools to minimize viral spread?).
Prompt 6: You say that men who have sex with men should “Limit the Number of Partners”. Would 365 partners per year be a sensible limit?
ChatGPT gives a rambling response that includes “Quality Over Quantity: Engaging with partners you know and trust may reduce risk.” and “Regular screening is essential but becomes logistically challenging with such a high partner count.”
Prompt 7: What’s your best guess as to a sensible number of partners, assuming that the partners are screened for mpox and that these are high quality partners (people that the man who has sex with men knows and trusts)?
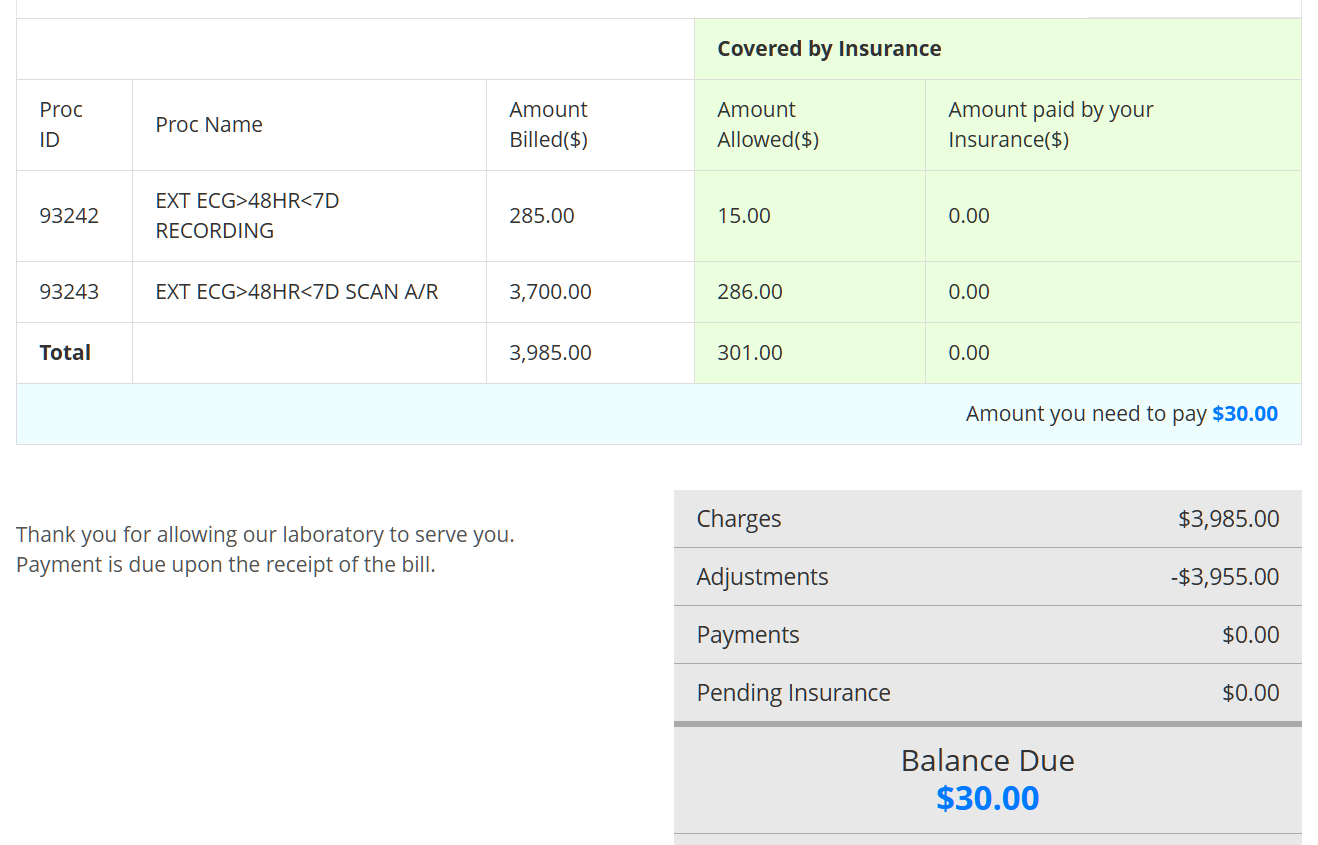
The full response below says that 50-100 sex partners per year is a sensible lifestyle when trying to avoid mpox infection and obtain “meaningful connections” with those sex partners.
The “sensible” number of sexual partners is subjective and depends on individual circumstances, preferences, and the quality of risk-reduction practices. If partners are screened for mpox, and relationships are built on trust and open communication, a more moderate number of partners would generally balance health and personal satisfaction while minimizing risks.
Factors to Consider
- Screening and Trust:
- Regular screening for mpox and other infections reduces risk significantly.
- Knowing and trusting partners helps ensure mutual openness about symptoms, exposure risks, and health status.
- Frequency of Contact:
- The number of partners should align with your ability to maintain safe practices (e.g., vaccination, symptom monitoring) and your emotional and physical capacity.
- Public Health Context:
- During active mpox outbreaks, even with high-quality partners, limiting the number of partners reduces overall exposure.
A Sensible Number
A reasonable estimate might range from 1 to 2 partners per week, translating to 50–100 partners per year under optimal conditions (e.g., vaccination, trust, and symptom screening). Here’s why:
- This frequency allows for meaningful connections and sufficient time to assess and manage any health risks.
- It strikes a balance between an active sex life and maintaining lower cumulative risk.
Key Takeaways
The number itself is less important than the quality of interactions and the consistency of risk-reduction practices:
- Stay vaccinated against mpox and other preventable infections.
- Monitor for symptoms regularly.
- Communicate openly about health and risks with partners.
By prioritizing safety and communication, individuals can maintain an active sex life while minimizing health risks.
Related:
- “Man likely spread monkeypox at Texas bathhouse through sex with multiple men” (the haters at the New York Post)
- “Spain monkeypox cases tally reaches 30, mostly linked to sauna” (Reuters, 2022): “The word sauna is used in Spain to describe establishments popular with gay men looking for sex rather than just a bathhouse.”