Week 4 of Internal Medicine clerkship, same team. Monday is call day. Our team is responsible for divvying up admissions to the hospitalist service. Our team has a low census (only about 6) after all the discharges so we’ll admit 6 patients today. I take the first admission. A 93-year-old female with Alzheimer’s and vascular dementia and COPD (chronic obstructive pulmonary disease) presenting via EMS (ambulance from the nursing home) for worsening shortness of breath. Typically, the medical student is tasked scouring through the 40-page stack of medical records sent from the nursing home for prescription medications. Fortunately, her three children, one granddaughter, and a great granddaughter are present to give a full history of her health. Her daughter: “She never smoked a cigarette in her life.She got COPD from second-hand smoke; her husband was the chain smoker.” Tiffany: “Now you see the challenge with the elderly. If they don’t live near family, it can be a crisis. Her past medical history is an enigma. We don’t know her goals of care, or if she already has a living will.”
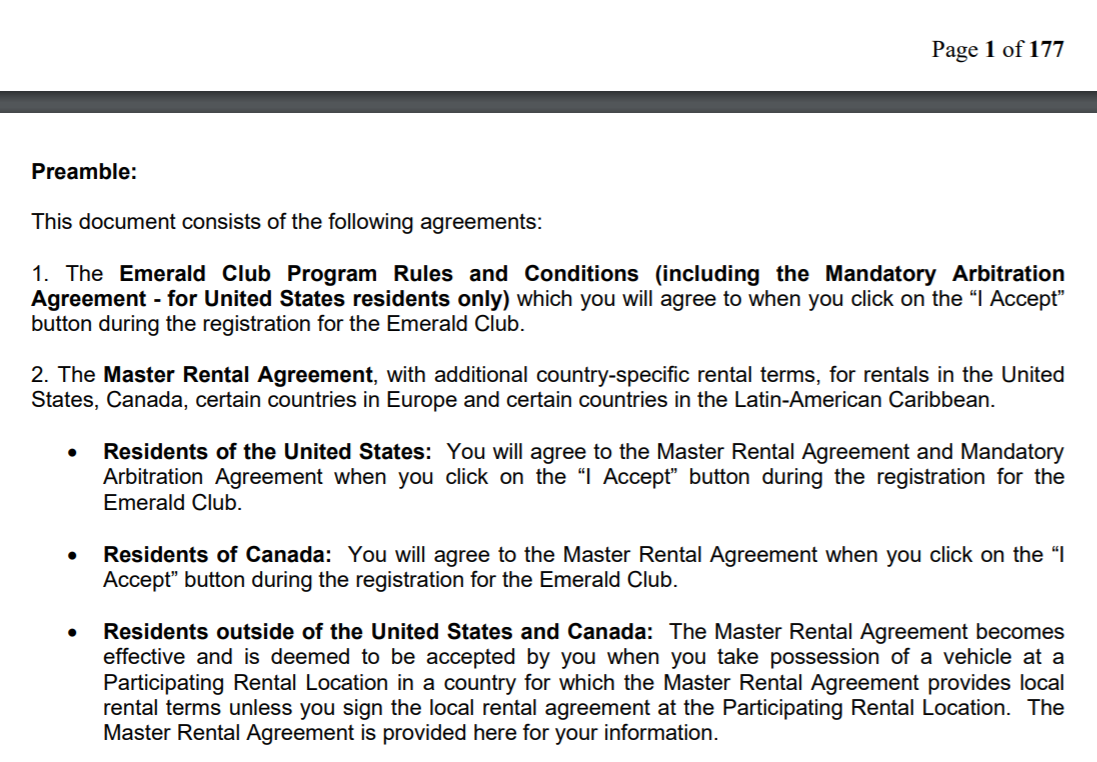
Her wheezing is audible from the hallway, but she is oxygenating well on 2 liters NC (2 liters oxygen delivered via nasal cannula prongs). We step out into the hall and explain her GOLD Stage 4 COPD (most severe) to her family members. She arrived in actual (as opposed to coding gimmick) respiratory failure. She has a severe acute respiratory acidosis with chronic metabolic compensation shown by ABG (arterial blood gas sampling). We avoid intubation by giving back-to-back DuoNeb nebulizer treatments until IV methylprednisolone (steroid, similar to cortisol) kicks in (about 30 minutes). We order a BiPAP (bilevel positive airway pressure) machine from the resident lounge. Briana emphasizes as we wait for the elevator, “BIPAP is never used unless there is a foreseeable improvement from a specific intervention — when in doubt, intubate. It is the safest intervention.”
We head up to the resident lounge to type H&P into Epic. Two hours later, we meet the attending, Formal Frank, in the ED to present our admissions. Sylvester describes a newly diagnosed lung cancer patient. Diane presents an undifferentiated pericardial effusion (fluid around the heart). In the room with my patient, the attending notes her inability to speak more than two words and that she is using accessory muscles (e.g., between ribs or in the neck) to breathe.
Formal Frank asks the granddaughter, “What is her baseline?” A great-granddaughter responds, “This isn’t her, she’s a stubborn old bat, but she’s as sharp as a whip. She remembers small details from our childhood. Right now she doesn’t even know who I am.”
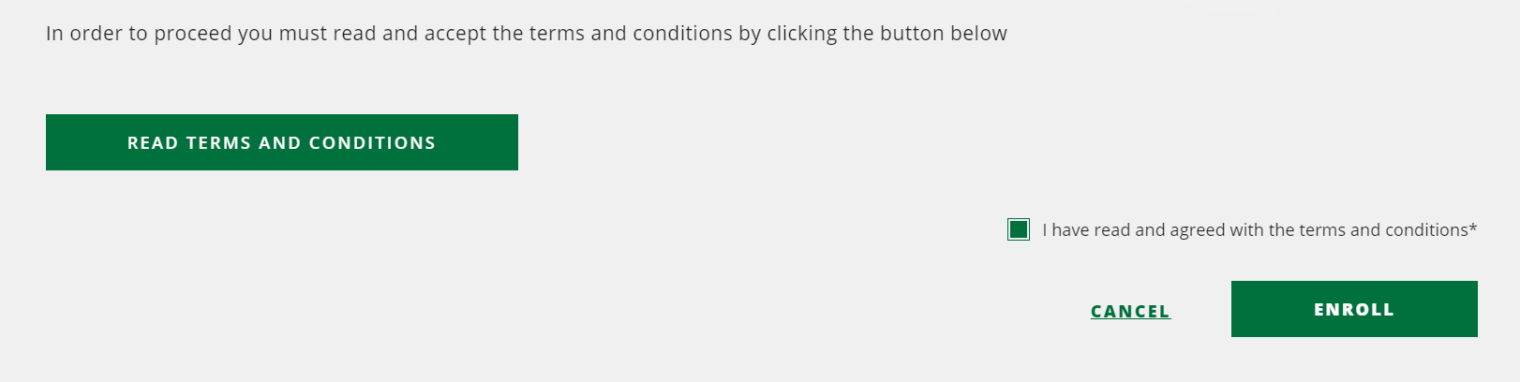
Formal Frank asks us, “You ordered BIPAP, but is she using BIPAP?” We stare at each other. “Just because you put something in the computer doesn’t mean it happens. Nurses think of our orders more like recommendations.” He had guessed right. Due to a combination of our patient improving and her dementia, the respiratory therapist had apparently given up after setting up the ($2000 billed to Medicare) machine.
As far as I could tell, the 45-year-old granddaughter stayed in the room for the entire five-night stay. She worked from her laptop and phone and slept in the recliner chair. Every time a nurse came in, she would ask what the next step would be. She related her concerns about the nursing home. “Her medications are ordered PRN [as needed]. That becomes an excuse for them not to give them,” says the granddaughter. “Their nurses are lazy, not like the ones you have here.” I work with the granddaughter on an updated list of medications, including an inhaled steroid for the GOLD stage 4 COPD.
My next admission is a 22-year-old patient with two-day history chest pain. A CT angiogram performed in the ED showed a pulmonary embolism. She also has numerous skin lesions. She has clear moon facies (swollen “moon face”) from steroids used for immune system suppression since age 9, when she received her first kidney transplant.
We get a deeper medical history from the mother, although she did not know the cause of the initial kidney failure. Either the kidney biopsy that would be standard today was never done or the mom can’t remember the result (or was never told). After all of the billions of dollars spent on electronic medical records, we’re forced to rely on the memory of laypeople for a continuous history of anyone who has been seen at multiple institutions.
We restart the patient’s immunosuppressive medications and start her on a heparin infusion for therapeutic anticoagulation.
I present the patient bedside to Formal Frank and Boss Bianca. The patient doesn’t have any questions, and we go into the hall to discuss. Formal Frank: “This is an exciting case! Think of everything this could be. What could cause a PE?” Sylvester, Diane, and I can’t come up with anything other than a run-of-the-mill PE from a DVT. Bianca: “Dig Deeper! People on immunosuppression are at a 100 times risk of developing cancer. She could have a nephrotic syndrome that causes you to be hypercoagulable. People with kidney transplants are at increased risk of glomerulonephritis. She’s also on a fibrate, maybe she has a heart attack.” (We don’t get to explore these issues, unfortunately. The patient’s shortness of breath resolves and she is discharged after two days to resume her job at Subway and see her outpatient specialists.)
On Thursday, Boss Bianca corrals the three of us after rounds. We head to the supply room, tucked away in the labyrinthine basement, to get several punch biopsies. “I have a surprise for you.” A patient admitted overnight to a different team may have syphilis. The 26-year-old relapsed on meth two weeks ago after his girlfriend left him. He has had several ulcers, largest in diameter about 4 cm and 1 cm deep, pop up on his body, including on his forehead, elbow, wrist, and back. “Look at me. I can’t go to work or anything.” We each choose a location and perform a punch biopsy. Later, I checked his chart and the syphilis tests came back negative. A dermatology consult did not result in a definitive diagnosis, but noted the possibility of an immune reaction to meth, possibly a necrotizing vasculitis?.
[Editor: Parents of couch-bound Xbox-playing youth nationwide should use this guy as an example. Even a meth head had a girlfriend and was passionate about going to work.]
Bianca and I run upstairs for a code blue for a 80-year-old DNR (“Do Not Resuscitate”) who is scheduled for transcatheter aortic valve replacement on Friday. He went asystole (flatline EKG). Boss Bianca instructs a nurse to get basic labs, a 12-lead EKG, and to get her the family’s phone number. “DNR does not mean do nothing. Check glucose, hypoxia, treatment arrhythmias.” She taps my shoulder to look at his Cheyne-Stokes breathing pattern. He would take 4-5 deep breaths, then stop breathing for several seconds. Bianca speaks to the daughter and explains the situation that he is DNR, and therefore no further interventions are indicated. The family understands, and says that they knew this was likely and that the valve replacement was extremely risky. Bianca instructs Tiffany to call the surgeon and tell her that the patient is dead.
[Editor: Medicare would have paid over $60,000 for the valve replacement, had the patient survived long enough to receive it.]
Friday is the medical students’ “24-hour” shift, from 6:00 am until morning rounds on Saturday (i.e., about 9:00 am). We work with our normal day team with rounds, followed by notes in the resident lounge. We attend a few procedures on our patients, e.g., endoscopy for GI bleeds, and then join the night team at 6:00 pm.
The chief resident functions essentially as an attending. She was asked to stay for an additional “chief” year following PGY3. She and I head to the med/surg floor to perform paracentesis (“tapping the belly”) on two patients with alcoholic cirrhosis.
[Editor: The good news that I learned at Harvard Medical School in 2019 is that these patients are not “alcoholics.” At worst, they are suffering from “alcohol use disorder.”]
I use an ultrasound to locate a pocket of fluid on a 35-year-old alcoholic cirrhosis patient with a belly swollen from ascites. She is animated, intelligent, and sober following two days of detox. It is tough to imagine that she is on disability and suffering from end-stage liver disease. I locate a pocket that is clear of bowel and mark it with a pen. My chief then preps and taps the belly. We get 4 liters, four test tubes of which we send to the lab for albumin ascites gradient (SAAG) to determine if there is portal hypertension or an inflammatory process.
The chief lets me do the next one, on a 65-year-old former alcoholic. After sticking a needle into the belly, advancing the catheter, and retracting the needle. The patient feels better after 2 liters, but we keep going until we’ve extracted 10(!). We increase his IV fluids to compensate for the expected dehydration.
We are beginning to fade at 1:30 am, fighting over who will get stuck with the next patient rather than who will get the privilege of taking the next one. The chief sends us home at 3:00 am. Sylvester and Diane both sleep at the hospital in the medical student call room. I decide to go home for 2 hours before returning for Saturday morning rounds at 7:00 am. I finished my notes before heading home so I leave after rounds and sleep.
We get the rest of the weekend off.
Jane had an exciting week on inpatient gynecology. A 65-year-old patient presented with stage 4 cervical cancer and necrotic tissue in the vagina. She’d been having regular checkups with a nurse-practitioner who ordered labs and assumed that the patient was seeing a Ob-Gyn and getting standard-of-care Pap smears. The doctors were outraged that this had been missed and now this otherwise healthy patient was sentenced to death.
[Editor: Although this patient plainly would have benefitted from screening tests, there is debate about whether the U.S. standard of care is the right one. See “Harms Of Cervical Cancer Screening In The United States And The Netherlands” (Habbema, et al. International Journal of Cancer 2017, 140:5): “Our main finding is that harms occur much more frequently in US than in NL, while the levels of incidence and mortality have been quite comparable between the two countries…” (the Netherlands screens at only about half the rate of the U.S. and only for women 31-60)]
Jane is exhausted and sore when she returns home. She spent five hours total driving the uterus with a uterine manipulator. “I was pushing so hard, my feet were slipping, but they kept saying, ‘Harder. Harder. Lift the uterus.’ Afterwards my hands were shaking. I could barely squeeze.” She continued, “And of course they then asked me to suture. They thought I was really nervous, but actually I was having trouble gripping the instruments.”
Statistics for the week… Study: 6 hours. Sleep: 5 hours/night; Fun: none.
The rest of the book: http://fifthchance.com/MedicalSchool2020
Full post, including comments