Here’s Bernie Sanders giving a “Let’s Go Brandon” speech on behalf of a mayoral candidate in Chicago. “All of us are sick and tired of the greed of the real estate speculators, of Wall Street, of the big money interests.”:
Not surprising that Bernie supports a fellow progressive, of course, but…
I wonder if there is a particular religious or ethnic group associated with the above categories of humans: speculators, Wall Street, big money.
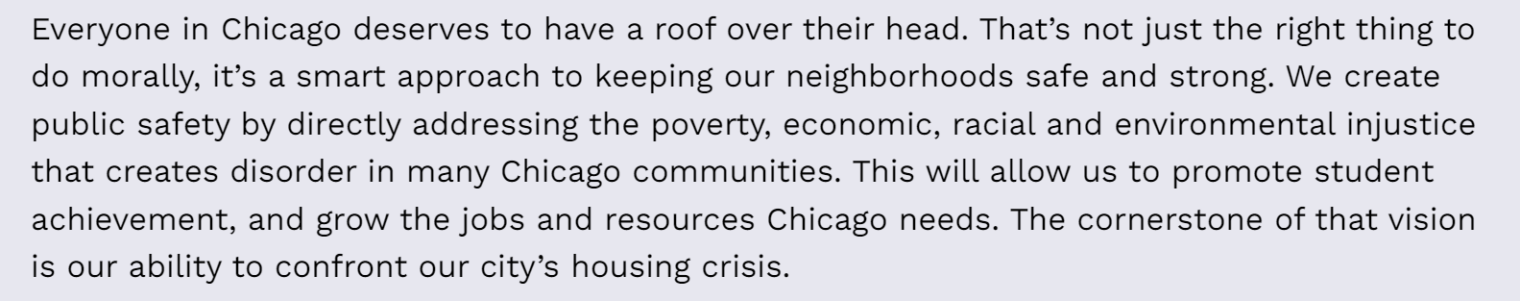
Separately, what a great day it would be for Florida realtors if Brandon Johnson can win the race in Chicago! He promises to give a free house to everyone who wants or needs one:
The wealthy will pay their fair share:
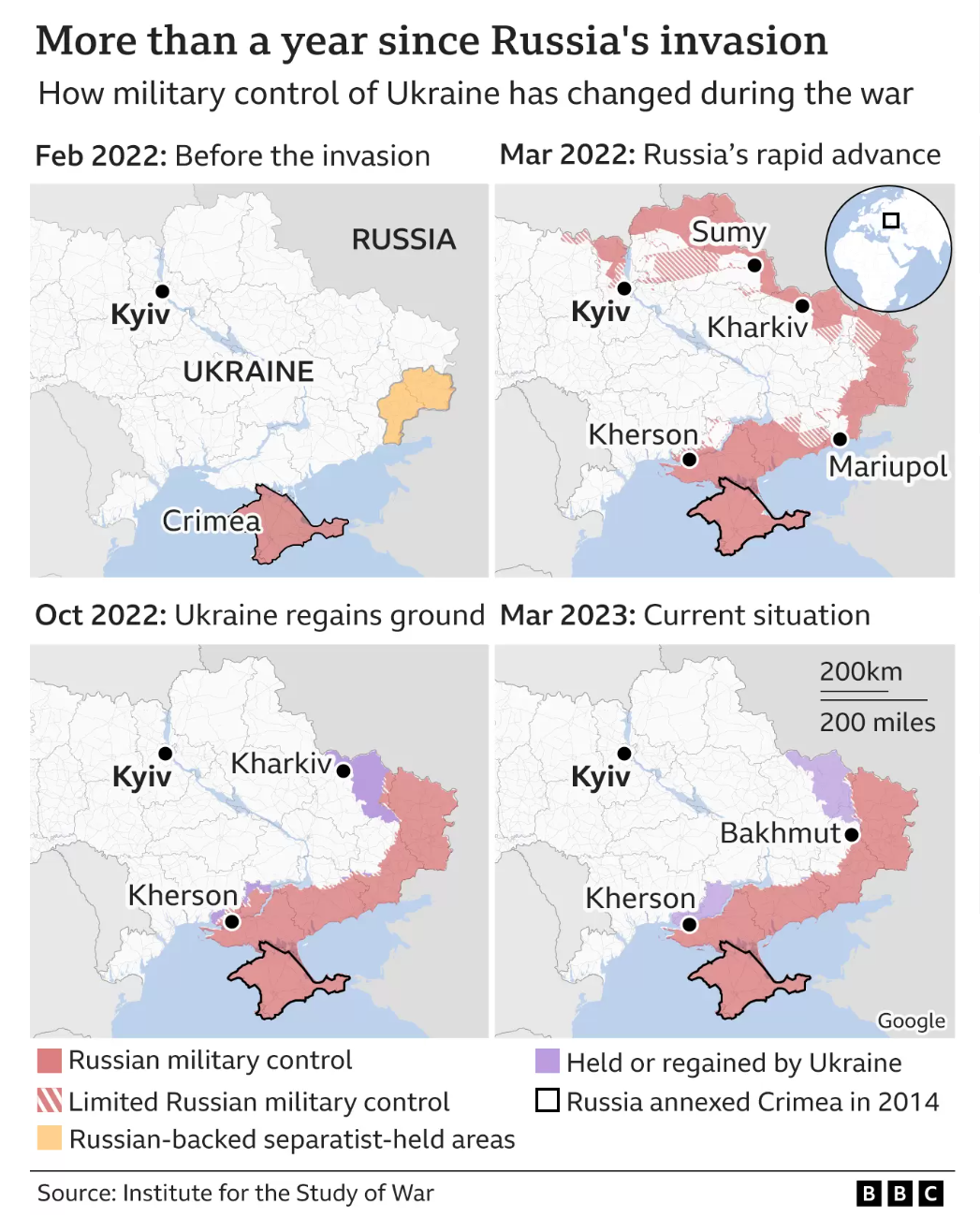
(but maybe some will move to our neighborhood instead? We already have a greedy real estate developer from Chicago two houses over (his company shut down all development in Illinois in favor of Florida in 2021). The local real estate hiccup seems to be over. Houses that sat on the market for 6 months have finally sold and new houses are selling in as little as 5 days, though the pace is nowhere near as frenzied as a year ago when only spectacularly stupid people were bidding against each other for houses. In nominal dollars, prices are about the same at the high end of the market and down 15-20% from the peak for peasant-class buyers ($1-2 million range).)
Everyone except cisgender males will be taken care of:
Florida and Texas can tell undocumented migrants that a whole world of services is theirs for the asking in Chicago:
Pregnant people in Florida who want abortion care after the 15-week limit (or maybe it will soon be 6 weeks) can fly nonstop to ORD and receive reproductive health care right in the terminal:
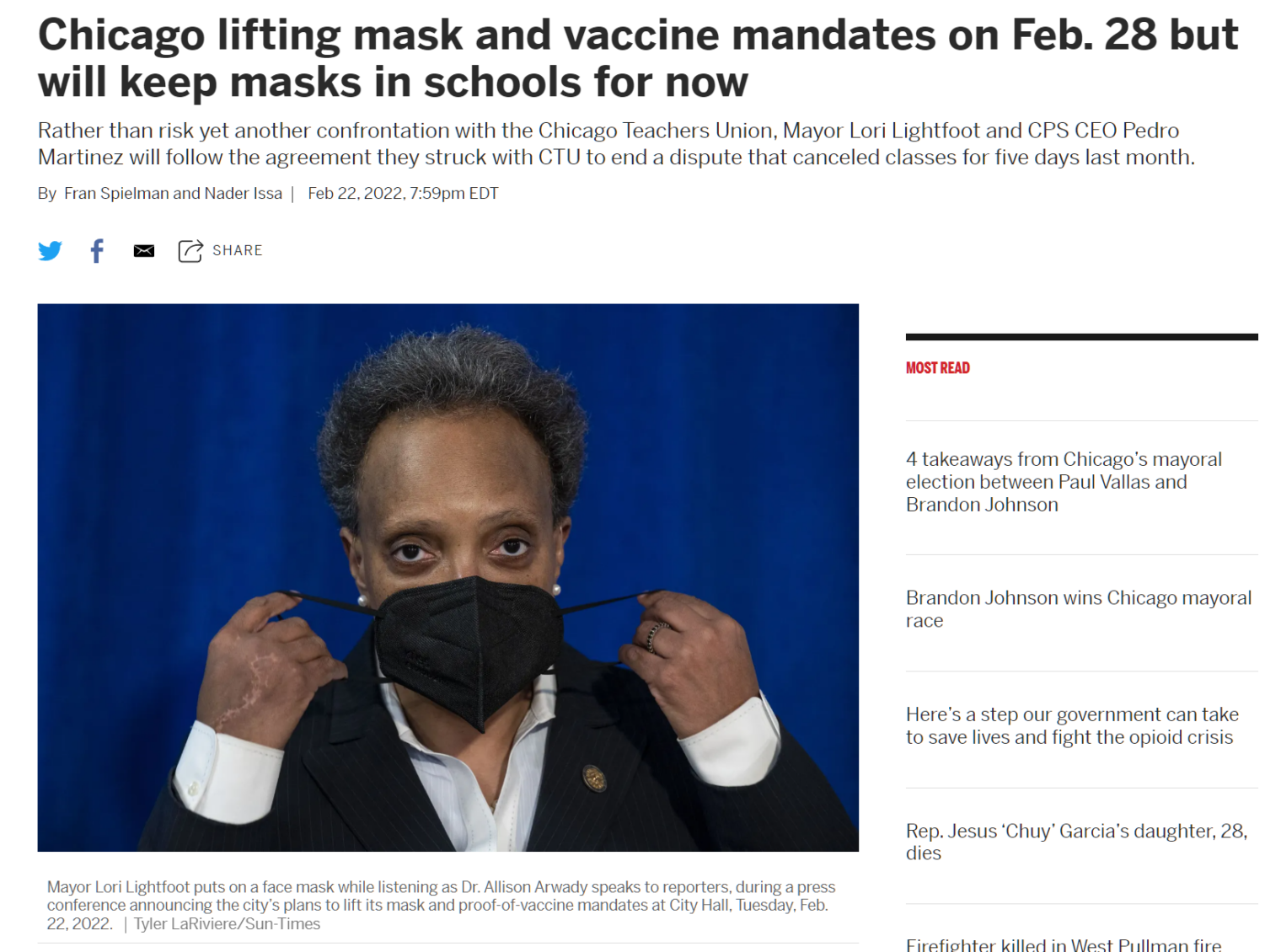
Let’s see if Brandon can win!
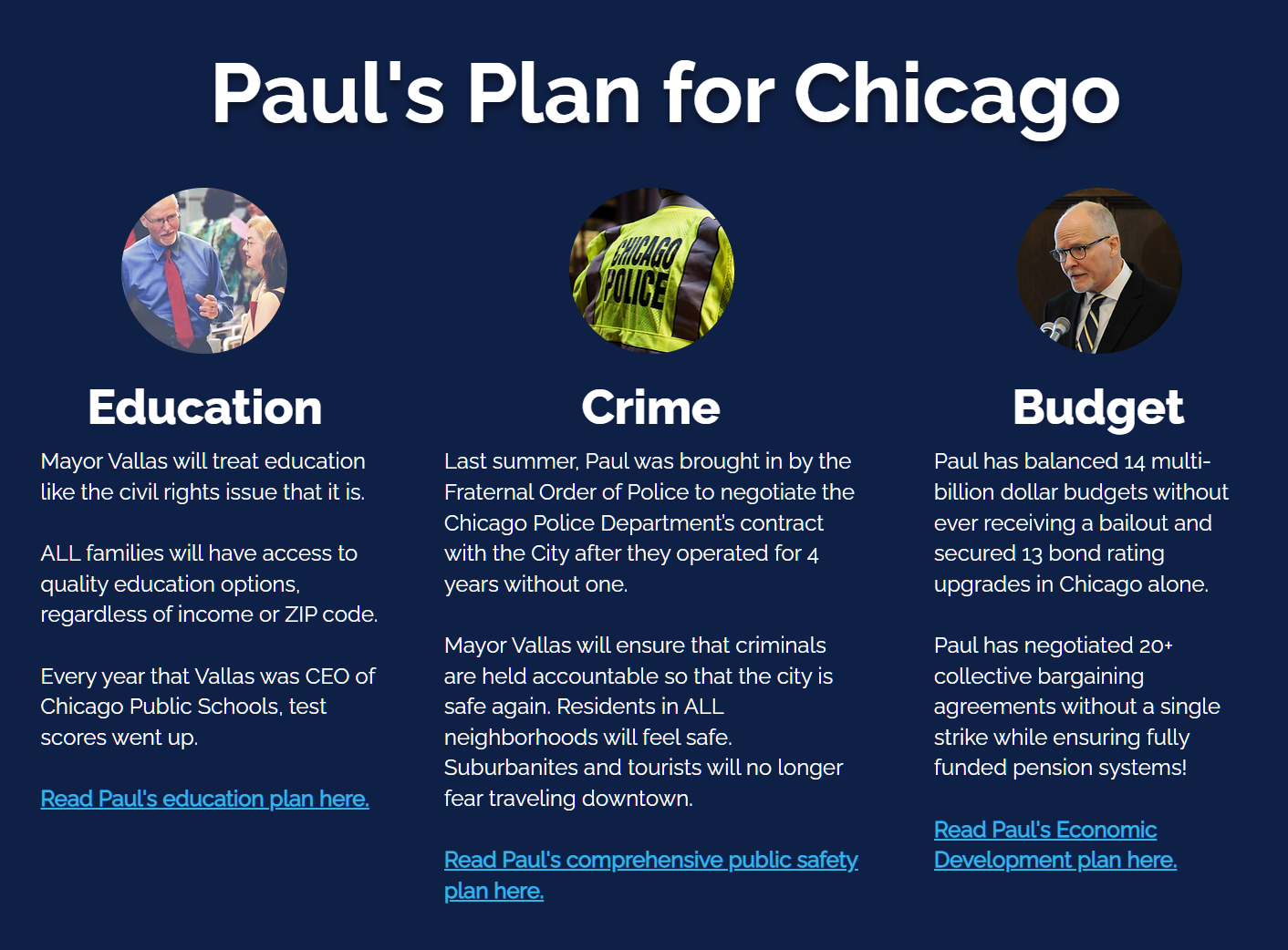
Who is against him? Paul Vallas, #OldWhiteGuy (but not a fossil like Bernie or Joe Biden).
Mr. Vallas is also a Democrat and is also passionate about expanding abortion care. Instead of saying that housing is a “right” for the unhoused and non-working, he says “chronic homelessness is almost never simply an issue of housing”. But, confusingly, he also says that it is about the housing:
Implementing a housing-first orientation and response that emphasizes permanent housing, with the right level of services, as the goal for people experiencing chronic homelessness.
He doesn’t say anything about immigrants, documented or otherwise. He is worried about the pension funds:
But why worry? As long as Democrats control D.C., won’t cities that can’t pay pensions, nearly all of which are run by Democrats, simply get bailed out by Congress and/or the Fed? The Feds have bailed out private pension commitments, e.g., from GM to the unionized workers. “The Coming Biden Bailout of Blue States and Cities” (WSJ, April 2, 2023):
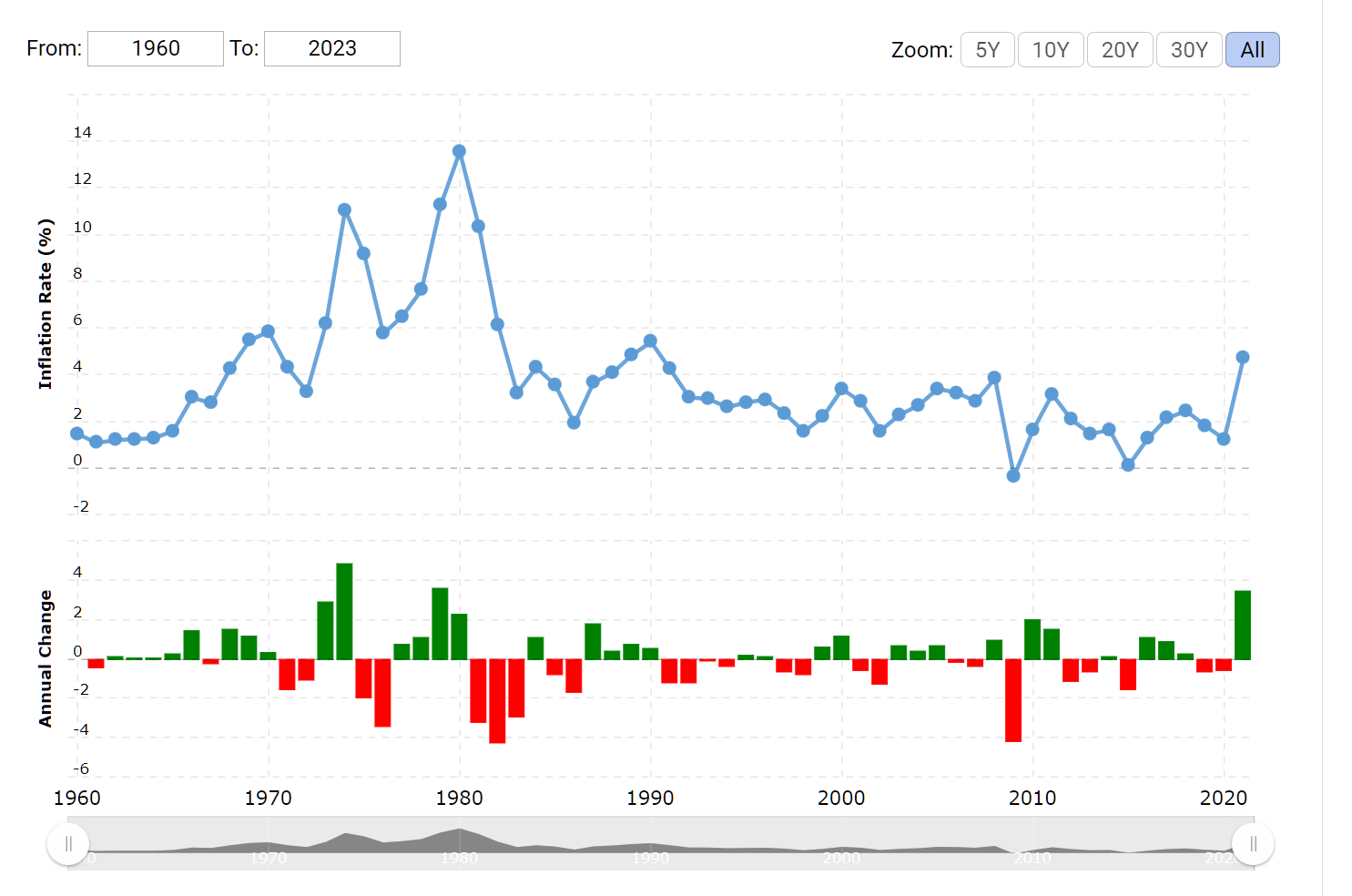
The Federal Reserve’s latest interest-rate hike paired with the continuing bank panic is causing credit conditions to tighten. State and local governments could be the next sinking ships that Washington gets called on to rescue.
The balance-sheet risks for mismanaged states and municipalities have been hiding in plain sight just as they were at Silicon Valley Bank. Continued financial-market turmoil and a prolonged economic downturn could cause some pension funds to collapse and cities to declare bankruptcy. Taxpayers will invariably wind up on the hook for politicians’ bad financial bets.
The most likely outcome: A cascade of bailouts by some combination of U.S. taxpayers, the Fed and municipal bond investors. Democratic-run states and big cities are simply too politically important for the Biden administration to let fail.
Putting more money into a pension fund when a federal bailout is on the horizon seems dumb, like a middle class family saving for college when the financial aid formula will just scoop up all of the savings by setting a higher price than if the family had spent it all on lavish vacations.
Readers: Who will join me and Bernie in denouncing “the greed of the real estate speculators, of Wall Street, of the big money interests”? And are you hoping for one candidate to prevail in Chicago? If so, which one and why?
Full post, including comments