From my inbox:
An Explanation of Benefits (EOB) has been posted to your *** Plan online member portal. To log into your account and review your explanation of benefits (EOB):
Go to https://****.com/login
Enter your Username (email address) and Password
Click on the Claims tab at the top of the page, choose claims.
Member claims are listed by date, with the most recent claim appearing at the top of the list. To view an EOB, click on the claim you want to view, then click on the pdf icon under View EOB.
(name hidden to protect the guilty)
So an Explanation of Benefits is available from my vaccine shot? Let’s actually log in…
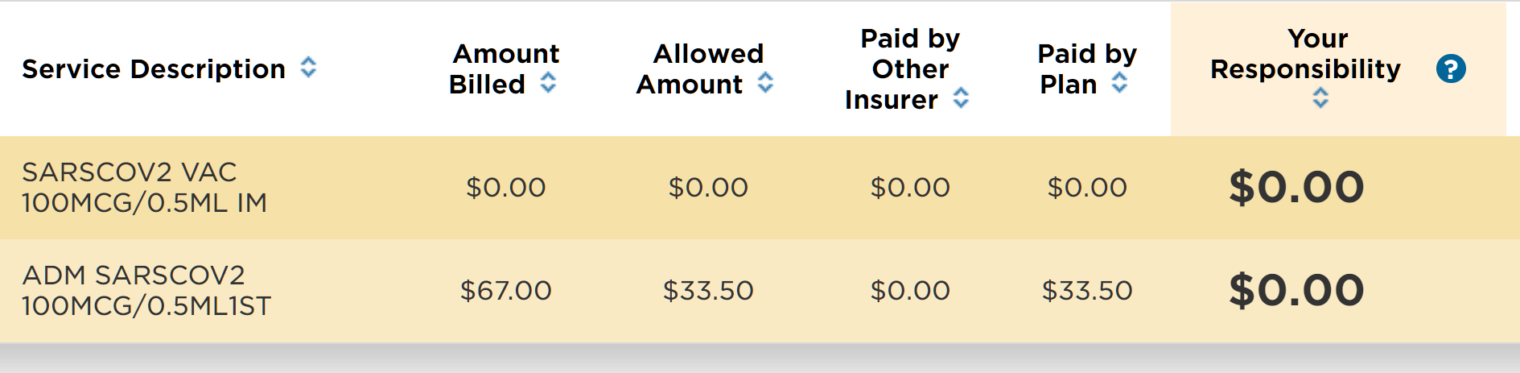
Even if the promised Explanation of Benefits did not exist, there was a page devoted to my Moderna shot. Two claims hit the insurer’s computer systems, one for $0 (the vaccine itself? Which Donald Trump arranged for the government to pay for?) and one for administering the vaccine:
The actual price is $33.50 to deal with me? But why bill $67? This is one of those rare situations in which there is no way to cheat the uninsured by hitting them with 2X or 5X the “negotiated” price that 98% of customers pay.
(Separately, I’m not sure how $33.50 makes this profitable for the clinic. They paid someone to build a web site where I could register and schedule, paid for a receptionist to check me in, paid an RN to ask me some medical questions, paid for a place where I could sit for 15 minutes after the vaccine, paid for people and systems to send this $67 bill to the insurance company, etc. Unless the Feds are giving them additional money for each shot, why do they want to be in this business?)
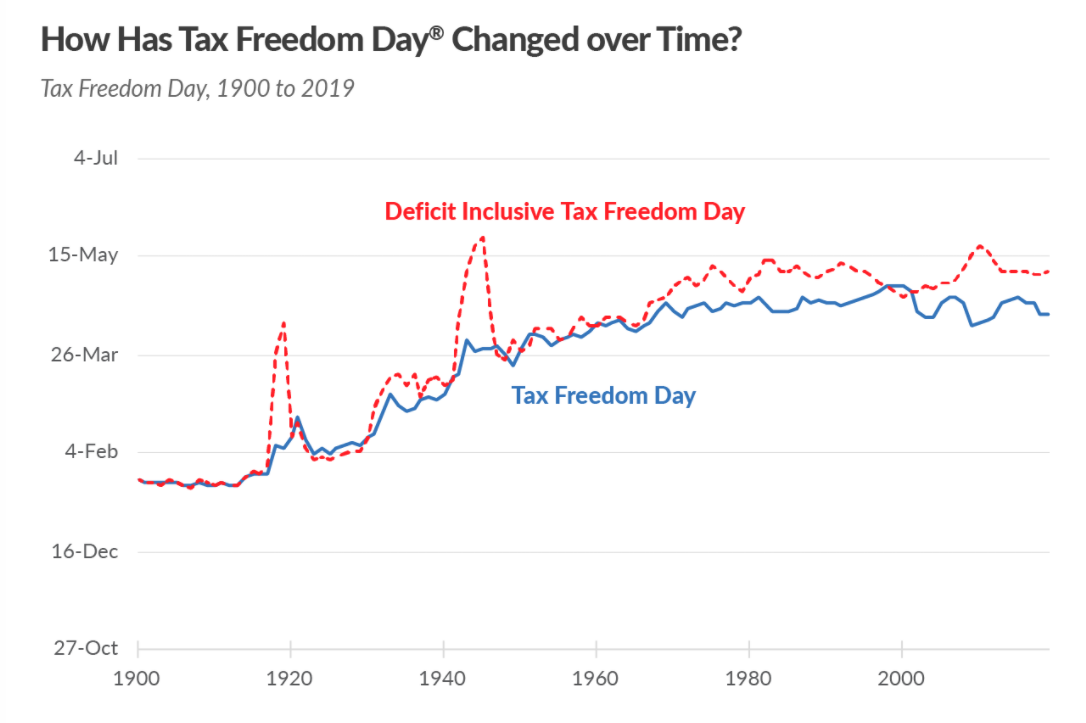
I wonder if the goal of the American health insurance system is to make our federal tax system seem logical, clear, and simple. Happy Tax Freedom Day to everyone! (filing is extended this year to May 17 #BecauseCoronapanic)
Note that Tax Freedom Day, on which you stop working for the government (pay all of those government workers who sat home for the past year!) and begin to work for yourself varies from state to state. It is May 3 in New York, April 23 in Maskachusetts, and April 20 in California. It was April 5 in Texas and April 4 in Florida. Before World War I, Tax Freedom Day was in January:
As best historians can tell, the American colonists-turned-rebels-and-traitors were paying roughly 2 percent of their total income for all taxes. So they achieved Tax Freedom about one week into January while complaining that being British subjects was oppressive (the Brits, meanwhile, were shelling out huge $$ to fight with “Indians” on all of the borders).
How about going forward? If Presidents Biden and Harris spend $1.9 trillion every few months on coronapanic Band-Aids, would the “deficit inclusive Tax Freedom Day” move to mid-summer, or, for those here in MA, into foliage season?
Full post, including comments