“Stanford president to resign following findings of manipulation in academic research” (CNN):
Stanford University President Marc Tessier-Lavigne said on Wednesday he would resign from his post after a review by a panel of scientists concluded that research papers he contributed to contained “manipulation of research data,” according to a report released by a special university committee.
His resignation, which was announced in an open letter to the school, will be effective on August 31, though he will remain on the Stanford faculty.
The last part is my favorite. Involvement with academic fraud is intolerable in an administrator, but acceptable for an active researcher and teacher. (Note that CNN implies in the headline that he will be gone (“resigned” from Stanford) when, in fact, he is merely moving offices.)
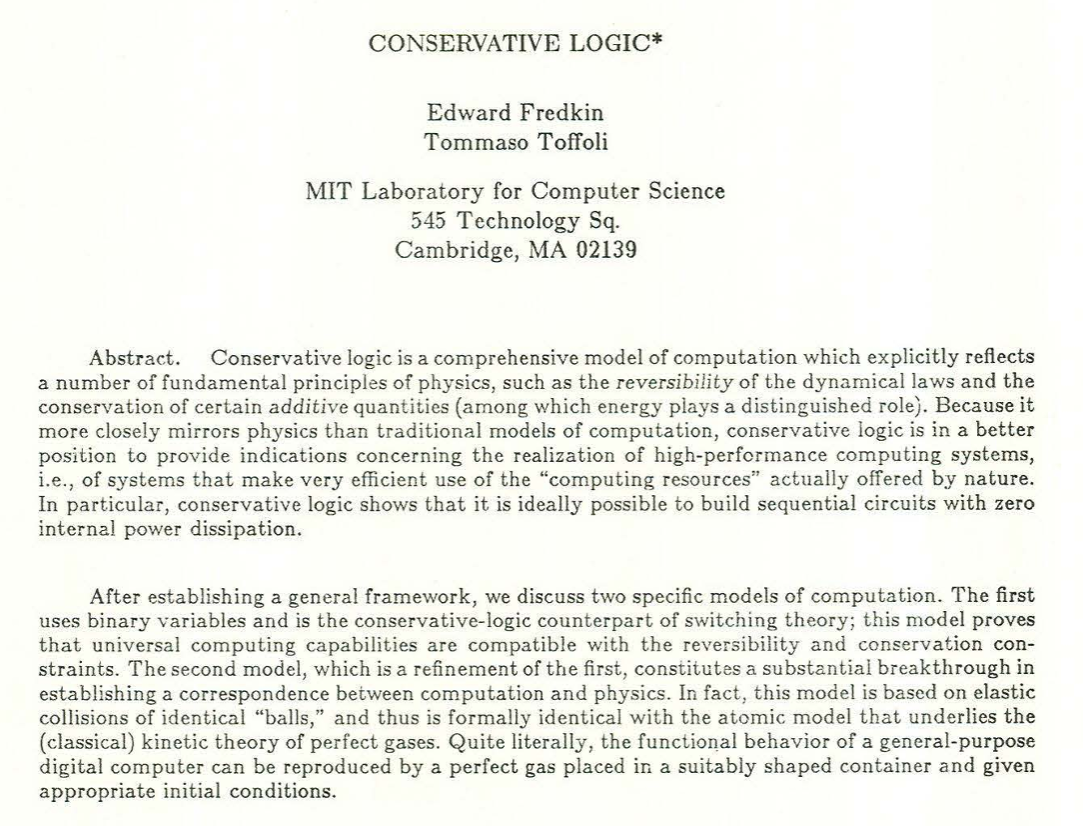
Maybe there is more to this great man than academic fraud. Let’s see what we can find with The Google…
August 2020, requiring ID to be displayed when walking outdoors on campus (but requiring ID for voters is hateful?):
The Campus Zones, which encompass research facilities and student housing on the east and west sides of campus, along with the Athletics Zone and the Campus Arts Zone, will also be reserved for approved Stanford community members at this time. … One notable adjustment for students, faculty, staff and postdocs approved to be on campus is a new requirement that they visibly display their Stanford IDs beginning on Sept. 8… You’ll be able to choose how to display your Stanford ID but recognizing that neck lanyards are already a common feature in our campus landscape, the university will be providing them to anyone who needs one to comply with this requirement. It’s also important to emphasize that the focus of the zones program is educational and health-promotional, not punitive. We’ll largely be focusing on signage that helps educate visitors about the temporary limits on access to campus. Safety personnel will be available in some of the areas in the campus zones that are currently most visited by members of the public to help educate them about the role of this program in supporting everyone’s health and safety, and to ensure we are all doing our part to comply with state and county guidance intended to prevent the spread of COVID-19.
January 2021, noting that the “best interest of students” is to not go to school in person:
As Persis and I communicated to students on Saturday, with great regret we had to change our plans to have the frosh and sophomore classes return to campus for the winter quarter, which was planned for two weeks from now. As we explained, the decision was triggered by the continuing surge in COVID-19 cases, which is now predicted to significantly lengthen the stringent public health restrictions we are under, which in turn are expected to seriously constrain the on-campus undergraduate experience for the better part of the quarter. We are deeply sorry to make this change of plans, but we believe it is in the best interest of students and our whole community.
From the same message, don’t forget to fill out the “Health Check” daily, even if injected with a medicine that at the time was sold as preventing infection by SARS-CoV-2:
As we begin this new year, we have reason to hope that, with vaccine distribution underway, we will begin to put the pandemic behind us in 2021. But while there’s promise of a new dawn on the horizon, we remain in a dark and difficult time. We all need to continue to protect ourselves and one another by practicing physical distancing, wearing masks, using Health Check daily for those on campus, and adhering to the other public health measures put in place to protect our community. This includes those in our community who have already been vaccinated.
Also from January 2021, deploring what the Deplorables did:
the violent mob attack on the Capitol Building was shocking and deeply troubling for all who respect our country’s democratic traditions and the peaceful transfer of power. It is a stark reminder of the vulnerability of our democracy, and the need for each of us, as citizens, to rededicate ourselves to upholding and defending our democratic values, norms and institutions.
Less well known, perhaps, is that the statement explains that this promotion also involves, in words so apt to the current moment, “… teaching the blessings of liberty regulated by law, and inculcating love and reverence for the great principles of government …”
In the same message that says paying students are not at liberty to show up on campus, he celebrates “liberty regulated by law”.
June 2023, in which it turns out that following the “law” is actually bad, e.g., if the law prevents you from discriminating on the basis of race:
I am deeply disappointed by today’s U.S. Supreme Court ruling that upends the long-standing practice of race-conscious university admissions to help achieve a diverse student body. I know that many of you in our community are disheartened. Now, our task is to respond in ways that allow Stanford to continue expanding opportunity and fulfilling our mission in a diverse and changing world.
Stanford has long supported race-conscious admissions as a means of obtaining the educational benefits of a diverse student body.
He’s proud to have been doing something for a long time that was found unconstitutional! And he further promises to violate the spirit of the Supreme Court ruling if it can be done in a way that doesn’t violate the letter:
Stanford will continue seeking, through legally permissible means, the broadly diverse student body that will benefit your educational experience and preparation for success in the world, and that will benefit our mission of generating knowledge.
September 2021:
Stanford is launching its first school in more than 70 years. This year has brought catastrophic weather events around the world, including another record-breaking fire season here in California. The extreme weather has underlined the urgency of the climate crisis, which has the potential to transform not only our planet, but also the health and well-being of humanity.
(But it isn’t an “existential crisis” as Joe Biden and the NYT say?)
What does the fraudster say about matters 2SLGBTQQIA+? It’s tough to know. The university’s main Twitter feed seems to have been silent on the subject of Pride all through June 2023. Instead they did things like celebrate the notorious hater John McEnroe:
Why is McEnroe a hater? State-sponsored NPR pointed out that Serena Williams was, as a purely factual matter, the best tennis tennis player in the world. McEnroe responded, “if she played the men’s circuit she’d be like 700 in the world.” There was some backlash… (Vox, for example)
Full post, including comments