A friend, who was forced to abandon his $10 million custom-built house in San Francisco after the wife refused to continue to live in a neighborhood where people injected heroin in their driveway, recommended San Fransicko.
I rejected the recommendation at first because I don’t have any intention of moving to the Bay Area or even visiting. See Working in San Francisco today (2019), in which I quote an understated young colleague:
[the meeting is] inside of WeWork Civic Center on Mission between 7th and 8th wedged between a homeless encampment and emergency heroin detox center. I would recommend picking a hotel in another part of town. … Due to the layout and direction of the one way streets and traffic I’ve found cabs/Uber to work fairly poorly and often take longer than BART. I stopped using cars when junkies started trying to open my door at stop lights.
But the book turns out to be more widely relevant. First, the author proves that a conservative is a liberal who has been mugged:
In the 1990s I had worked on a broader set of progressive causes, including advocating for the decriminalization of drugs and alternatives to prison. But for most of the last two decades my research and writing has focused on the environment. And, in the early summer of 2020, I was busy running my nonprofit research organization and preparing for the release of my book on the topic. It was anarchy of a different sort that motivated me to write San Fransicko. During the pandemic, a growing number of people in floridly psychotic states were screaming obscenities at invisible enemies, or at my colleagues and me, on the sidewalks or in the street, as we went to and from our retail office in downtown Berkeley, near the University of California.
Though I have been a progressive and Democrat all of my adult life, I found myself asking a question that sounded rather conservative. What were we getting for our high taxes? And why, after twenty years of voting for ballot initiatives promising to address drug addiction, mental illness, and homelessness, had all three gotten worse?
Inspect the lamppost before parking your Tesla Model S Plaid:
Complaints about human waste on San Francisco’s sidewalks and streets were rising. Calls about human feces increased from 10,692 to 20,933 between 2014 and 2018. In 2019, the city spent nearly $100 million on street cleaning—four times more than Chicago, which has 3.5 times as many people and an area that is 4.5 times larger. Between 2015 and 2018, San Francisco replaced more than three hundred lampposts corroded by urine after one had collapsed and crushed a car.
(Car and Driver: “trust us, you don’t want to do 200 mph in [the Tesla S Plaid]. Even 162 mph was terrifying, wandering and nervous to the point that we were concerned about our ability to shepherd it between lane lines. The steering doesn’t firm up enough with speed, making the task more difficult. At similar velocities, a Taycan is resolutely stable. Another reason to fear a 200-mph speed is brakes that got soft during our testing.”)
The author points out that Californian taxpayers give “people experiencing homelessness” and “persons with substance use disorder” (CDC preferred terms) everything that is required to survive until death by overdose:
Progressives give homeless people the equipment they need to live on sidewalks. After Occupy Wall Street protests were held in Oakland’s City Center in 2011, protesters gave their tents to the homeless and money to buy more.8 Five years later, a graphic designer in San Francisco purchased and gave away $15,000 worth of camping tents. “Other organizations were giving them out as well,” noted the city’s head of homeless services in 2016, “and now we’ve got 80 encampments.” San Francisco remains significantly more generous in its cash payments to homeless, and other spending to serve them, than other cities. For example, San Francisco’s maximum General Assistance cash welfare monthly benefit for the poor is $588, as compared to $449, $221, and $183 for individuals in San Diego, Los Angeles, and New York City, respectively. While New York City, Chicago, Phoenix, and San Diego spend 3.5, 1.1, 0.9, and 2.5 percent of their budget on homelessness services, San Francisco spends 6 percent. When local, state, and federal funding are accounted for, San Francisco spends $31,985 per homeless person just on housing, not including General Assistance, other cash welfare programs like Temporary Assistance for Needy Families, and other services. By contrast, New York City spends $11,662 and Los Angeles spends $5,001.
San Francisco, according to the book, is the nation’s best destination for any would-be “Persons who returned to use” (CDC). The city and its array of homeless industrial-complex non-profit org contractors will supply “Persons who use drugs/people who inject drugs” with clean needles and crack/meth pipes in a location conveniently across the street from an open-air drug market.
For a bunch of rich say-gooders, San Franciscans are awfully stingy:
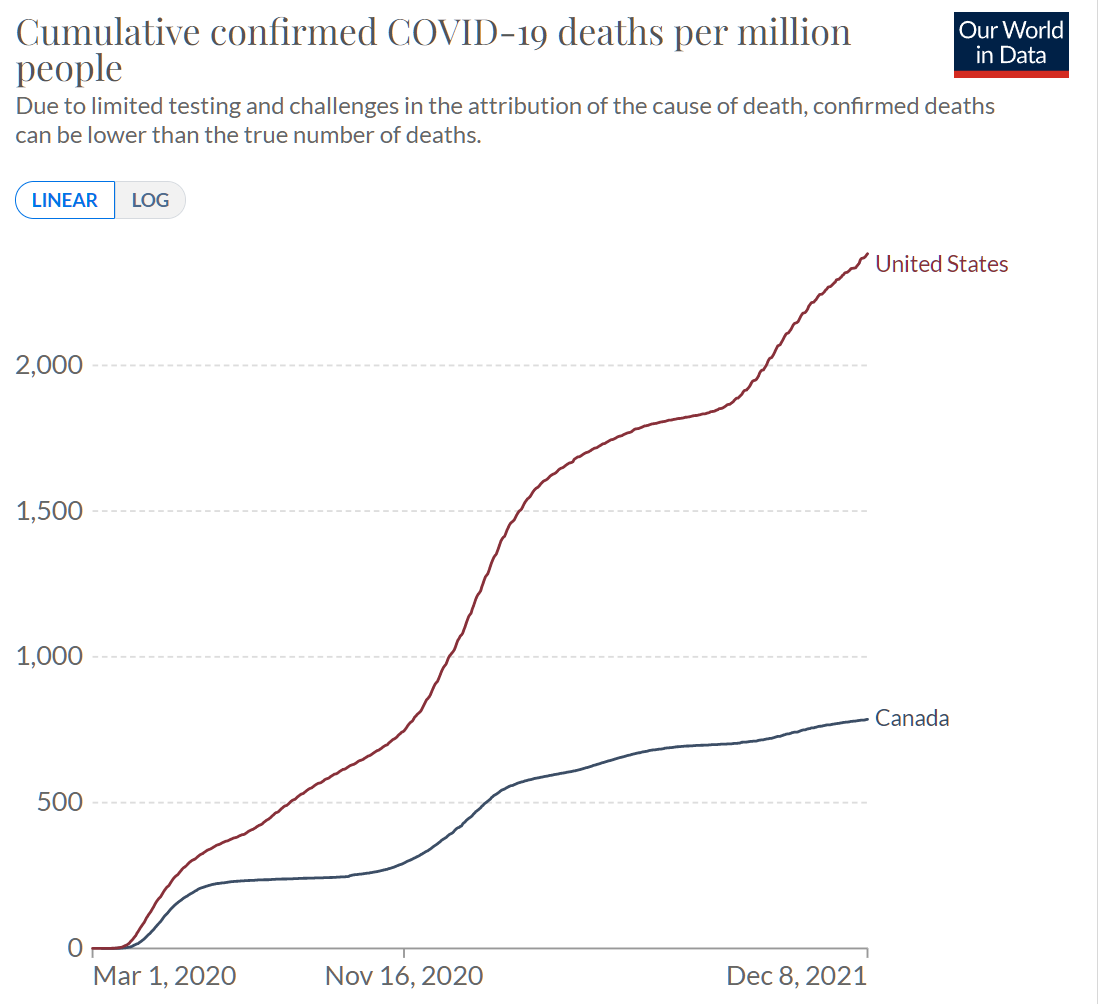
Mayor Breed said she opposed Proposition C because she feared that spending yet more on homelessness services, without any requirement that people get off the street, would backfire. “We are a magnet for people who are looking for help,” she said. “There are a lot of other cities that are not doing their part, and I find that larger cities end up with more than our fair share.” After San Francisco started offering free hotel rooms to the homeless during the 2020 coronavirus pandemic, first responders reported that people had come from across the state. “People are coming from all over the place—Sacramento, Lake County, Bakersfield,” said the city’s fire chief. “We have also heard that people are getting released from jail in other counties and being told to go to San Francisco where you will get a tent and then you will get housing.”
If housing is a human right and health care is a right and clean needles are a right and inequality is bad, why does San Francisco object to caring for the poorest and most addicted of Bakersfield? The San Francisco median household income is 2X what the good citizens (and undocumented!) of Bakersfield enjoy. Californians will cheerfully pay for every American’s abortion. “California plans to be abortion ‘sanctuary’ if Roe v. Wade is overturned”:
With more than two dozen states poised to ban abortion if the U.S. Supreme Court gives them the OK next year, California clinics and their allies in the state Legislature on Wednesday revealed a plan to make the state a “sanctuary” for those seeking reproductive care, including possibly paying for travel, lodging and procedures for people from other states.
Why is it objectionable to pay for housing the nation’s already-born unfortunates?
I’ve long been an advocate that the marginal tax rate should be 100 percent on incomes greater than my own and on wealth greater than my own. It turns out that the unhoused think along the same lines:
Even people who would prefer to live in sober environments say they do not want to quit their addictions. “When we surveyed people in supportive housing in New York,” said University of Pennsylvania homelessness researcher Dennis Culhane, “almost everybody wanted their neighbors to be clean and sober but they didn’t want rules for themselves about being clean.” In 2016, after the city of San Francisco broke up a massive, 350-person homeless encampment, dozens of the homeless refused the city’s offers of help. Of the 150 people moved during a single month of homeless encampment cleanups in 2018, just eight people accepted the city’s offer of shelter. In 2004, just 131 people went into permanent supportive housing after 4,950 contacts made by then-mayor Newsom’s homeless outreach teams.
How about the richest and goodest of the rich say-gooders?
In 2018, a reporter asked Marc Benioff if Prop C would create a magnet effect. “It seems like one of the things that you guys are doing is you’re creating a magnet for people to come to the city and be homeless,” she said, “because it’s not a hostile environment. Everybody has talked about seeing people out on the street openly shooting up.”
“That’s just not true,” said Benioff. “I can tell you that’s clinically not true. Our University of California at San Francisco, we’ve got the clinical studies to show you that when you give homeless people a home, their lifestyle does change.”
According to Benioff, #Science (“clinically”) proves that providing a house is the cure. What is Marc Benioff doing about it, relative to his net worth (estimated by The Google at $10.8 billion)? He could spend $9.8 billion on helping his brothers, sisters, and binary-resisters who are experiencing homelessness and still have “tres commas”. According to the developer that I talked to in Real estate peak near? (cost to buy a crummy old apartment building about the same as to build new), it costs about $130,000 “per door” to build medium-quality apartments. If Benioff spent his way down to “merely three commas” that would work out to 75,000 new apartments and, therefore, assuming a 2BR average size, 150,000 human lives transformed (more than double the entire unhoused population of San Francisco and Los Angeles combined). Where are “The Benioff Towers” in which the nation’s unhoused can be housed in peace and tranquility?
(Separately, it looks as though Mr. Benioff has not been persuaded by the “Black Girls Code” signs that are attached to the buses that circle his $1 billion office tower.
“Salesforce’s equality struggles burst into the public” (Protocol, 2/8/2021):
In a resignation letter posted to LinkedIn earlier this month, Cynthia Perry wrote a searing take-down of the company’s racial equality efforts, specifically the treatment of Black employees, at the massive software provider.
“I am leaving Salesforce because of countless microaggressions and inequity,” she wrote. “I have been gaslit, manipulated, bullied, neglected, and mostly unsupported … the entire time I’ve been here.”
[Salesforce’s] struggles with race and equality aren’t new. For one, its diversity statistics remain abysmal: Just 3.4% of its 49,000 workers identify as Black.
“Salesforce, for me, is not a safe place to come to work. It’s not a place where i can be my full self. It’s not a place where I have been invested in. It’s not a place full of opportunity. It’s not a place of Equality for All. It’s not a place where well-being matters,” she wrote in the letter posted on LinkedIn.
“Words must be followed up with action. And if they can’t be, then there should be no words,” she wrote. “There is a really big gap between how Salesforce portrays itself and the lived experience I had working at this company.”
Let’s hope that the above highlighted point is incorrect. Otherwise rich Bay Area residents could be in real trouble!)
What’s the story here in Palm Beach County? The median income is only half of San Francisco’s and there is no income tax, but funds are in ample supply due to property taxes on the mega-rich (soon those $80,000/year property tax payments will be 100% deductible from federal taxes!). The 2008 “Ten-Year Plan to End Homelessness in Palm Beach County” says that 1,766 people were homeless in 2007. The 2020 count was 1,510 (of whom 480 were sheltered).
Circling back to the opening sentence, what are the rich people who have continued to live in San Francisco doing? “San Francisco residents are hiring private security to patrol their streets in bid to stay safe, amid crime spike that has left many fearful of going outside during the DAY” reports the Daily Mail. And, indeed, my friend confirmed that this was the path his former neighbors were going down.
More: read San Fransicko.
Related:
Full post, including comments