“High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2” (preprint on cdc.gov):
Results show that the doubling time early in the epidemic in Wuhan was 2.3–3.3 days. Assuming a serial interval of 6–9 days, we calculated a median R0 value of 5.7 (95% CI 3.8–8.9).
In “Full range of coronaplague opinions” (March 25), I first noted that a team at Oxford led by Sunetra Gupta conjectured that as many as half of Britons were already infected with coronavirus due to the high R0. If the conjecture were true, it would invalidate the recommendations of the Imperial College study that led to a Western rich-country shutdown (except for Sweden). (No point in shutting down a society/economy to reduce transmission of a disease if the disease has already reached most people.)
When the Imperial College study leader upped his estimate of R0 to “just over three”, the scale of the deaths in the UK dropped by a factor of 10 (“Update on the coronapanic fueled by Imperial College”).
Can we believe this spectacular R0 number? It is lower than measles (12-18 without vaccinations). But such a high value seems inconsistent with the success of various Asian countries that have suppressed COVID-19.
Note that the authors of the new paper are huge fans of government and public health interventions:
Our results suggest that a combination of control measures, including early and active surveillance, quarantine, and especially strong social distancing efforts, are needed to slow down or stop the spread of the virus. If these measures are not implemented early and strongly, the virus has the potential to spread rapidly and infect a large fraction of the population, overwhelming healthcare systems.
But if they are right about R0, it is unclear how these could work in the U.S. once the economy and society are reopened. Consider a single infected traveler to an uninfected region of the U.S. A week after a visit to a business convention or a theatrical performance there could be more than 300 cases (45 infected at the first event, as with the choir practice in Washington; doubling to 90 after 2.5 days; doubling to 180 after 5 days; doubling to 360 after 7.5 days).
Also, if they’re right about R0, it is way too late for Sweden to do anything to change its trajectory. Our media are desperate for Swedes to die (today: “Sweden’s Relaxed Approach to the Coronavirus Could Already Be Backfiring” (TIME)), but since they didn’t shut down weeks ago the virus has to be pretty much everywhere by now. There wouldn’t be any point to Sweden falling in line with the sober non-science-denying governments.
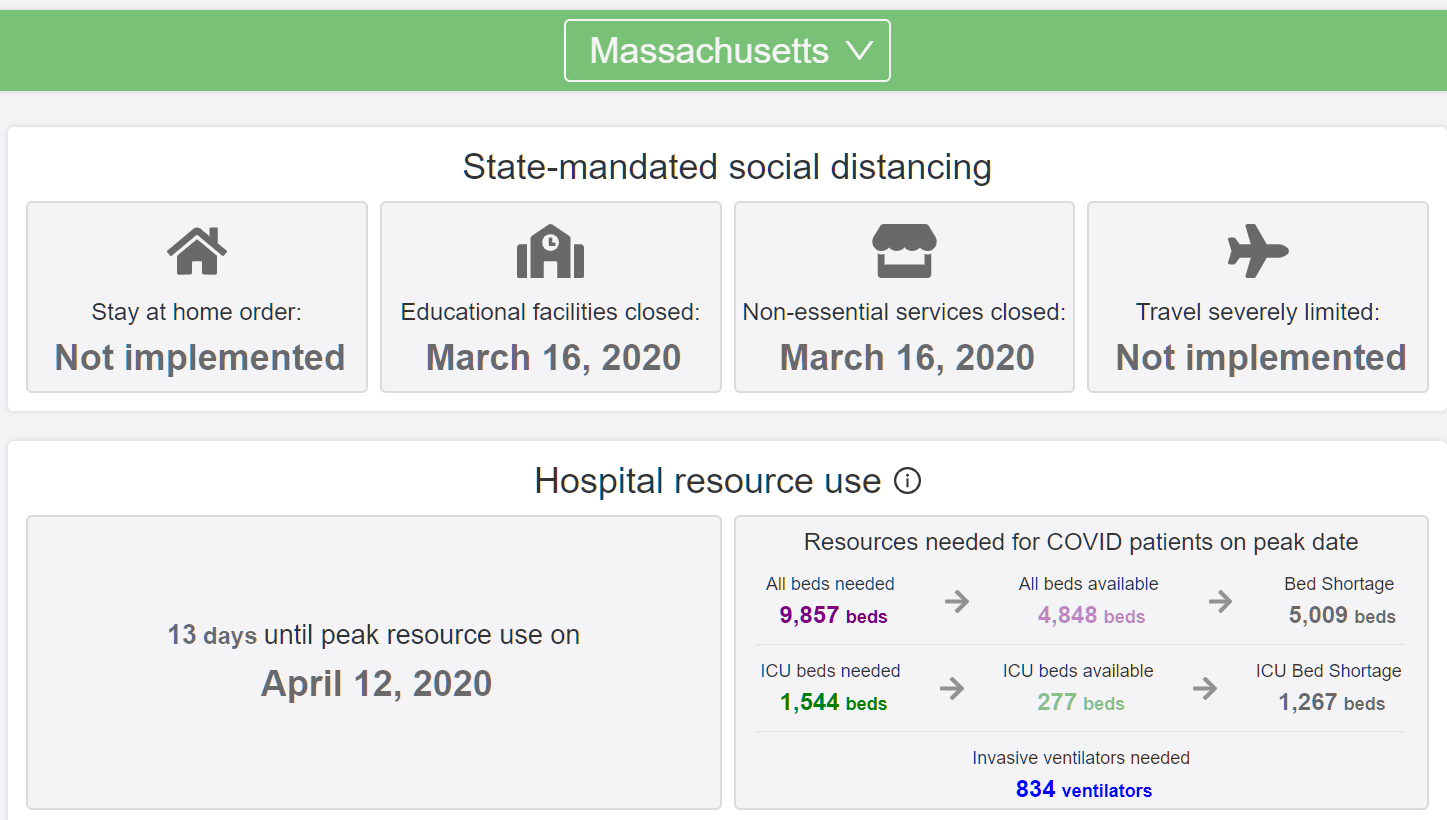
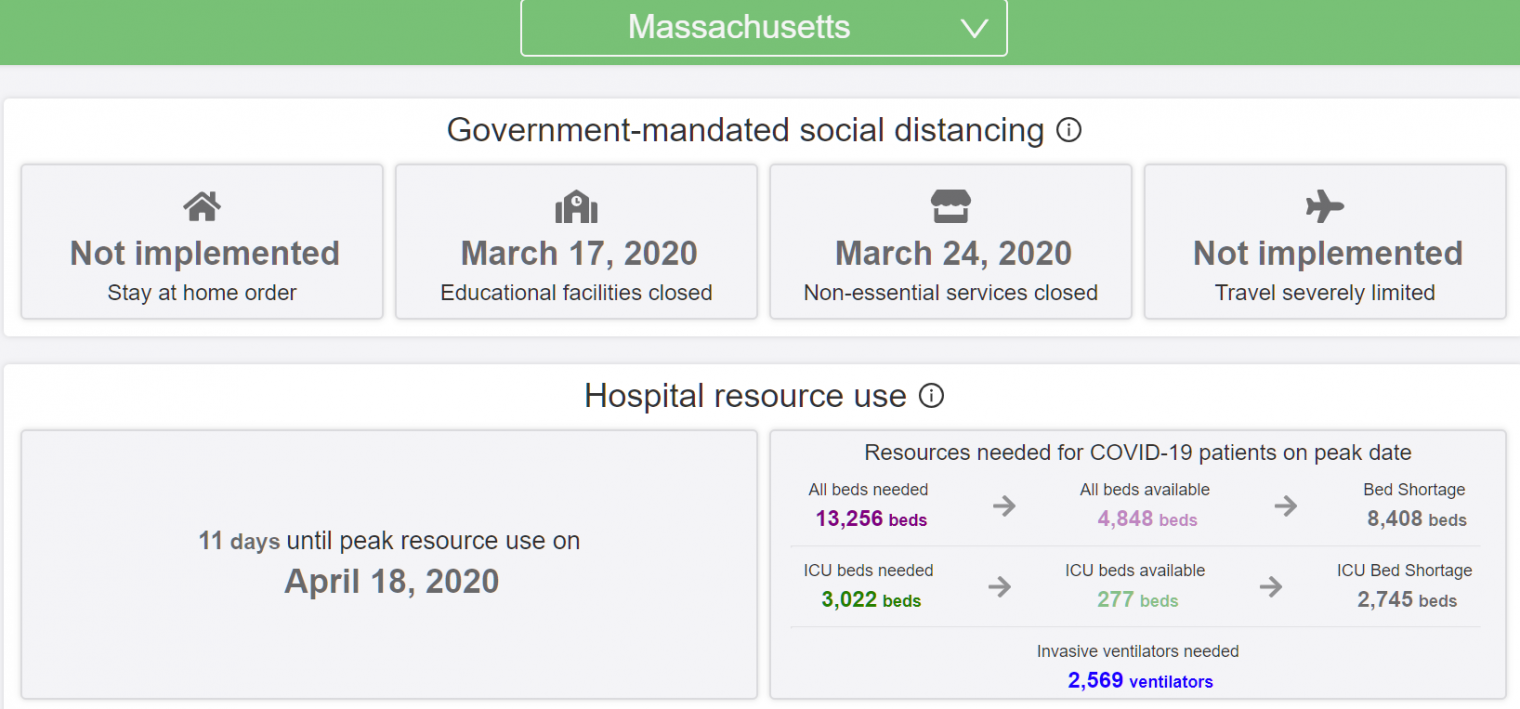
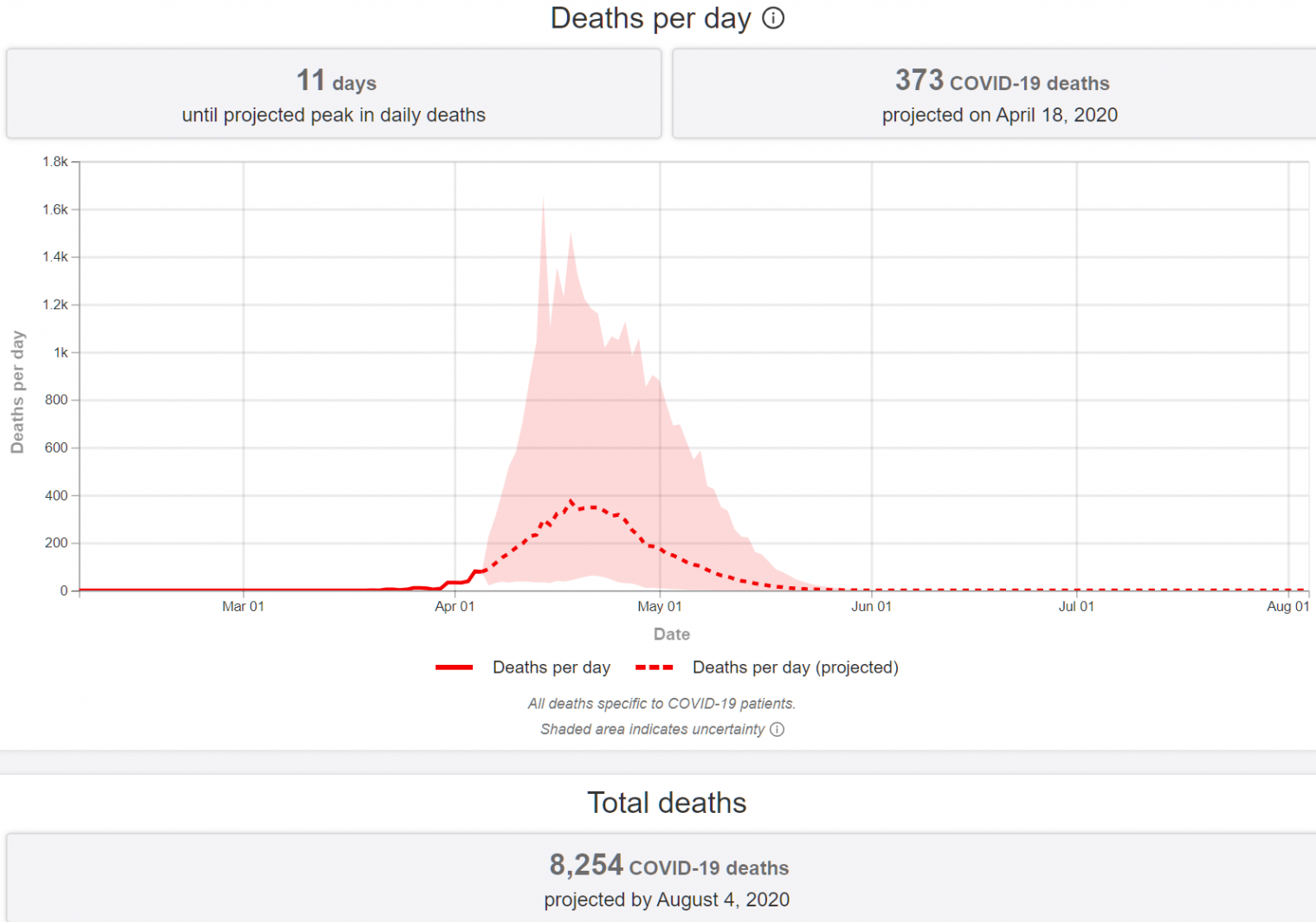
[Note that Sweden’s new case rate is lower than Massachusetts and the death toll is similar on a population-adjusted basis (10 million for Sweden; 7 million for Massachusetts). The current University of Washington deadpool forecast is 5,625 for MA and just 4,182 for Sweden (i.e., shut-down MA will see substantially more deaths per 1,000 residents than open-for-school-and-work Sweden). Somehow the deaths of thousands of Massachusetts residents after dramatic government school and business closures is not interesting. (I’m keeping the numbers up to date in this older post.)]
Why can’t we do a test of the general population? “Coronavirus may have reached Colorado as early as January” (Colorado Sun) If R0 is, in fact, 5.7, shouldn’t everyone in Colorado who is going to develop symptoms already have developed them? (The U Washington deadpool says that Colorado peaked yesterday for hospital utilization.)
Doing a super crude calculation, in which the doubling time stays constant, we take the base 2 log of Colorado’s population of 5.6 million. From a single infected person showing up, it takes just over 22 doublings for everyone to be infected. If the doubling time is 2.5 days, that’s 55 days (i.e., if the first infected person arrived in mid-January and the doubling time lengthened gradually (due to a lot of people already being infected), the 100-percent infected time would be right around now).
Or maybe a single R0 number is not that useful. R0 is high in China and U.S. urban mass transit environments such as New York and Boston, but much lower in sprawling car-dependent environments (e.g., Denver)?
Full post, including comments