Ron DeSantis and Coronapanic
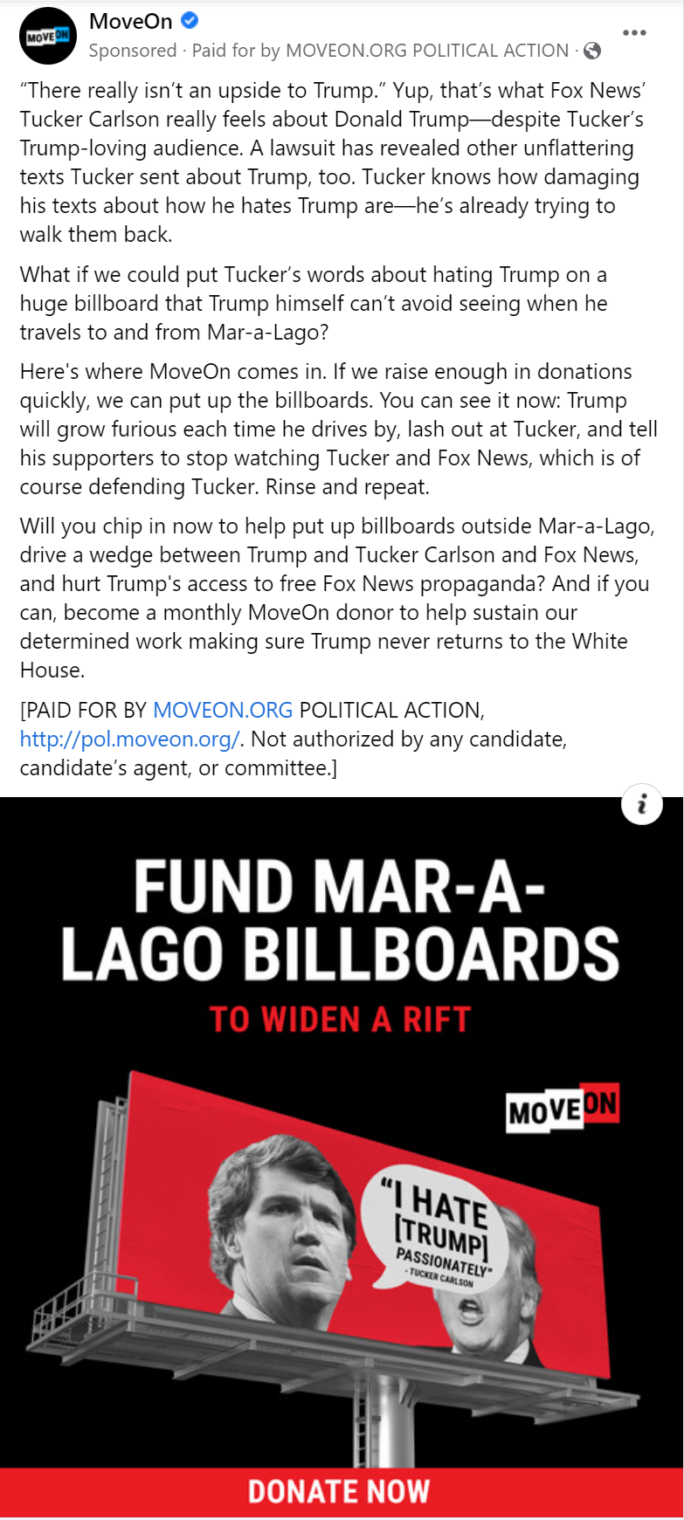
Posts so far regarding The Courage to Be Free: Florida’s Blueprint for America’s Revival, by Ron DeSantis:
Today let’s look at the chapter on coronapanic.
Compared to some of the Deplorables who comment here and myself, Ron DeSantis was a late convert to the Church of Sweden. He declared a state of emergency on March 9, 2020 and “Later than most governors, DeSantis imposed a lockdown” on April 1, 2020 (The Hill):
“All persons in Florida shall limit their movements and personal interactions outside of their home to only those necessary to obtain or provide essential services or conduct essential activities,” his order said.
The lockdown ended on April 29, 2020 and that’s when DeSantis began to diverge from the Faucists. The book downplays DeSantis’s one-month Faucist period to concentrate on his Church of Sweden rebellion. He opens by quoting Eisenhower:
“we must also be alert to the equal and opposite danger that public policy could itself become the captive of a scientific-technological elite.” [1961]
Eisenhower cited the alarming risk that what he termed a “scientific-technological elite”—an elite that is neither interested in nor capable of harmonizing all the competing values and interests that are the hallmark of a free, dynamic society—could commandeer policy and, ultimately, erode our freedoms.
Eisenhower wouldn’t have been surprised by the takeover of American society by the Covidcrats:
In March 2020, Fauci was held up as the authority on the coronavirus. On its face, this seemed understandable because Fauci was the head of the NIAID and touted as the nation’s foremost expert on infectious diseases. However, Fauci was also the epitome of an entrenched bureaucrat—he had been in his position since 1984, demonstrating staying power in Washington that would not have been possible without being a highly skilled political operator. He proved to be one of the most destructive bureaucrats in American history.
Ron describes getting immersed in the Imperial College London model and conversations with various high-level bureaucrats, including CDC director Robert Redfield, Deborah Birx, but perhaps not the Great Fauci Himself.
At one point, I asked Dr. Birx whether the policies for which the expert class was advocating—and which could be very destructive to society—had any precedent in modern history and, if so, what were the results. “Well,” she said, “this is kind of like our own science experiment.”
I decided that I needed to read the emerging research and consume the available data myself, not just about Florida or the United States, but also about what was going on in other countries.
I wanted to be armed with the foundational knowledge to chart my own course for the State of Florida. This course kept our state functioning and ultimately led to Florida serving as an example for freedom-loving people not just in the United States, but around the world.
As more data came in, it became clear that the Fauci policy of perpetual mitigation was wrong. One important insight stemmed from a study done by a team of Stanford researchers led by Dr. Jay Bhattacharya, a physician at the Stanford School of Medicine who also had a PhD in economics and was one of the few prominent academics willing to speak publicly about the failures in the COVID-19 policies advocated by Fauci and his followers. The Stanford study examined the prevalence of SARS-CoV-2 antibodies, which can be detected after someone recovers from a coronavirus infection, in Santa Clara County, California. The study found that the prevalence of antibodies in the population was dramatically higher than the number of “cases” that had been detected up to that point,
Ron DeSantis was checking the curves wherever he could find data:
The April 2020 COVID-19 wave in New York saw hospitalized COVID-19 patients peak at 18,000, a significant number but something that the medical system could handle and a far cry from the 140,000 predicted by the flawed models.
He got some information from a Deplorable Science-denying Nobel laureate in chemistry:
While lockdown advocates claimed the epidemiological curves nosed over because of so-called social distancing, Levitt pointed out how lockdown-free Sweden also saw its first COVID-19 wave perform in a similar fashion. Indeed, as successive COVID-19 waves hit various parts of the United States in the ensuing months, the waves almost always featured about a six-to-eight-week period during which the wave would escalate, peak, and then decline. This was true regardless of mandatory “mitigations” that were employed.
He makes similar points to what I wrote in June 27, 2020 in “Looking at Covid-19 death rate is like the old saying “An economist is someone who knows the price of everything and the value of nothing”?“
A Covid-19 epidemiologist can tell you how many Covid-19 deaths your society has suffered and, perhaps, some things that you can do to reduce Covid-19 deaths going forward. But the Covid-19 epidemiologist can’t tell you whether Intervention A against Covid-19 is actually worth implementing because (a) the Covid-19 epidemiologist is ignoring deaths from all other causes, and (b) epidemiologists in general can’t tell us what human activities are worth accepting some risk of death. How many lives are we willing to sacrifice in order that our children can go to school? Obviously we are willing to sacrifice some, because all of the driving of children, teachers, and administrators to and from school causes some deaths. But the threshold number at which schools should be shut down is not something that any epidemiologist can give us.
Is asking an epidemiologist whether to keep schools and playgrounds open like asking your accountant whether you should buy a dog? Yes, the expert can give you a bit of insight (“my other clients with dogs spend $4,000 per year on vet, food, and grooming”), but not a life-optimizing answer.
Here’s what Ron D writes:
So many of the so-called experts lost sight of the fact that true public health cannot be blind to everything but a single respiratory virus. Led by Dr. Fauci, the experts seemed to be throwing away previous understandings of how to approach pandemic management—and sowing fear and hysteria in the process.
The mostly peaceful mostly unmasked George Floyd mass gatherings showed Ron D that the Covidcrats weren’t serious about preventing Covid-19.
For two months, these so-called experts lambasted anyone for making a cost-benefit analysis when it came to COVID-19 mitigation policies. Then, the moment it suited their political interests, they reversed course by endorsing the protests as passing their cost-benefit analysis over COVID-19 lockdowns. That they specifically rejected protesting for other causes they did not support told me all I needed to know about what partisans these people were. These “experts” were not going to save us. People making the best decisions for themselves and their families would. It was up to leaders like me to lead in a way that was evidence-based, that recognized the obvious harms of mitigation efforts, and that best maintained the normal social functioning of our communities.
I’m still looking for good summary-by-state excess mortality data (comparable to what Our World in Data gives us by country), but Ron apparently ran the numbers and Florida has done pretty well by this metric (remember that the righteous said that Florida’s COVID-tagged death numbers were fabricated so excess deaths should be a better place to look):
Between April 2020 and mid-July 2022, New York witnessed an increase of so-called excess mortality of 20 percent, while California experienced an excess mortality increase of 17.7 percent. Excess mortality represents deaths above what is normally expected; of course, it includes COVID-19 deaths but also includes deaths caused by lockdown policies. During the same period, excess mortality increased in Florida by 15.6 percent—a smaller increase than in lockdown-happy states that typically received
Ron says that he doesn’t Deny Science. He just follows different scientists:
The approach that we took in Florida reflected the thinking of prominent epidemiologists like Stanford’s Jay Bhattacharya, Harvard’s Martin Kulldorff, and Oxford’s Sunetra Gupta.
And it is following these MDs, PhDs, and MD/PhDs that turned DeSantis into a Science-denier:
After several weeks of consuming data and measuring it against policies implemented around the country, I decided that I would not blindly follow Fauci and other elite experts. To this end, I revoked my order suspending elective procedures at hospitals. The predicted April surge in coronavirus patients never materialized, leaving Florida with one of the lowest patient censuses on record. I also abandoned the federal government’s framework of essential versus nonessential businesses. Every job and every business are essential for the people who need employment or who own the business. It is wrong to characterize any job or business as nonessential, and this entire framework needs to be discarded in pandemic preparedness literature.
It was easy for me to join the Church of Sweden because nobody cares what I think, say, or do. But Ron took a lot of heat:
When Florida experienced its first major COVID-19 wave starting in the middle of June 2020, it sparked massive media hysteria. The media drew a connection between Florida’s lack of restrictions and the COVID-19 wave. If only Florida had not been so reckless, the narrative went, it would not be experiencing such a wave.
After I saw other states from similar geographies endure similar COVID-19 waves in the fall and winter, I knew that COVID behaved in a seasonal pattern. I was, though, monitoring the data on a daily basis, and I was sure that the summer wave would follow a pattern similar to the trajectory that Dr. Michael Levitt had identified from earlier waves. It would not simply increase exponentially without end in the absence of a shutdown. The pressure grew on me to shut down the State of Florida to mitigate the COVID-19 wave, not just from the media but also from experts like Dr. Anthony Fauci and partisan opponents. On July 8, 2020, Dr. Fauci advised that states like Florida “should seriously look at shutting down.” This was because, Fauci explained, “we are seeing exponential growth.” All Democratic members of Florida’s US House delegation but one wrote me a letter to demand that I shut down the Sunshine State and impose a compulsory mask mandate. The letter was written on July 17, 2020.
Some of my friends and allies were worried about all the negative attention and urged me to implement some mandates and restrictions to help take the heat off me. For me, the important thing to do was to safeguard the freedom, livelihoods, and businesses of the people I was elected to serve. If doing so caused me to suffer political damage, and even to lose my job as governor, then so be it. It is easy to do the right thing when it is popular, but leadership is all about doing the right thing when under political attack.
In fact, by July 8, 2020—the day Fauci said Florida should shut down—infections in our state had already peaked. I knew this because visits to the emergency departments for COVID-like illness, which was the best leading indicator of infection trajectory, peaked on July 7.
What Fauci and especially the House Democrats were calling for was a post-peak shutdown, which would have been totally counterproductive and hurt Floridians.
As it turned out, even though during the summer wave Florida saw an increase in patients hospitalized for COVID, our hospital capacity was more than sufficient to handle the higher patient volume, just like in lockdown-free Sweden in the spring.
How did Florida end up as the mask-free state?
I was skeptical that masks would provide the protection that the public health establishment claimed, but I was adamant that a mask mandate was not an appropriate use of government power. If the masks were as effective as claimed, then people would choose to wear them without government coercion.
(The latest on Ron’s unscientific skepticism… “Were masks in hospitals a waste of time? Hated NHS policy made ‘no difference’ to
Full post, including comments