Argentina investor looks at another government that can’t resist spending beyond its means
A recent Wall Street Journal interview with a guy who made $billions in Argentine bonds… “Paul Singer, the Man Who Saw the Economic Crises Coming”. First, let’s check his track record as a prophet:
“Men and nations behave wisely,” the Israeli statesman Abba Eban observed, “when they have exhausted all other resources.”
In an interview for these pages in 2011, he warned about the broad discretion the then-new Dodd-Frank law gave government officials to deal with what they deem systemic risks. The “atmosphere of unpredictability” doesn’t “make the system any safer,” he said. “This is nuts to be identifying systemically important institutions.”
A dozen years later, he still thinks it’s nuts: “As we’ve seen with SVB and Signature, virtually any institution can be deemed systemically important overnight and seized, with the government then completely empowered to determine what happens to various classes of creditors.”
The result is to destroy market discipline and encourage bankers to behave recklessly. He recounts a conversation on the trading desk at his firm following the recent weekend of bank bailouts. “If they hadn’t guaranteed all the deposits,” a colleague said, “things would’ve gotten very ugly in the markets on Monday.”
Mr. Singer replied: “That is entirely true. Things would’ve been ugly. But is that what regulation is supposed to be? Wrapping all market movements in security blankets?”
What about the most significant economic phenomenon of the moment?
Mr. Singer saw inflation coming at the start of the Covid pandemic. “We think it is very unlikely that central bankers will move to normalize monetary policy after the current emergency is over,” he wrote in an April 2020 letter to investors. “They did not normalize last time”—meaning after the 2008 crisis—“and the world has moved demonstrably closer to a tipping point after which money printing, prices and the growth of debt are in an upward spiral that the monetary authorities realize cannot be broken except at the cost of a deep recession and credit collapse.”
Mindful of the history of the 1970s, when inflation retreated several times only to come roaring back, Mr. Singer figures short-term declines will convince policy makers that they’ve slain the beast. They’ll “probably go back to their playbook,” resuming the policy of easy money.
The guy’s remedy is one that will never fly with the American voter:
How do we chart a course back toward sound money and long-term prosperity? “The optimistic scenario,” Mr. Singer replies, “would entail pro-growth reforms across the board, including tax reductions, entitlement reforms, regulatory streamlining, encouraging energy development including hydrocarbons . . . cutting federal spending, selling the asset holdings on central bank balance sheets.”
(see quote from Abba Eban, above)
Let’s assume that Congress and the Fed are never going to change. How does an individual investor protect him/her/zir/theirself from the doom that Singer predicts? That’s where it gets tough! The guy is bearish on nearly all assets, especially crypto. His $55 billion Elliott Management fund can do things that none of us can do, e.g., buy a big stake in Salesforce and get the company to fire 10 percent of its employees to boost profits (and therefore stock value).
A friend who has done some co-investing with Paul Singer’s fund points out that “talk is cheap” and he won’t accept Singer as a prophet without evidence that he made huge money in inflation swaps after that April 2020 newsletter to his clients. Wikipedia points out that Singer was predicting doom in 2014:
In short, if this smart and experienced fund manager is right, U.S. and European assets will be eroded by inflation for the next few years and returns to investors will be minimal.
In a November 2014 investment letter, Elliott described optimism about U.S. growth as unwarranted. “Nobody can predict how long governments can get away with fake growth, fake money, fake jobs, fake financial stability, fake inflation numbers and fake income growth,” Elliott wrote. “When confidence is lost, that loss can be severe, sudden and simultaneous across a number of markets and sectors.”
Anyone who acted on that advice would have done quite poorly until 2022!
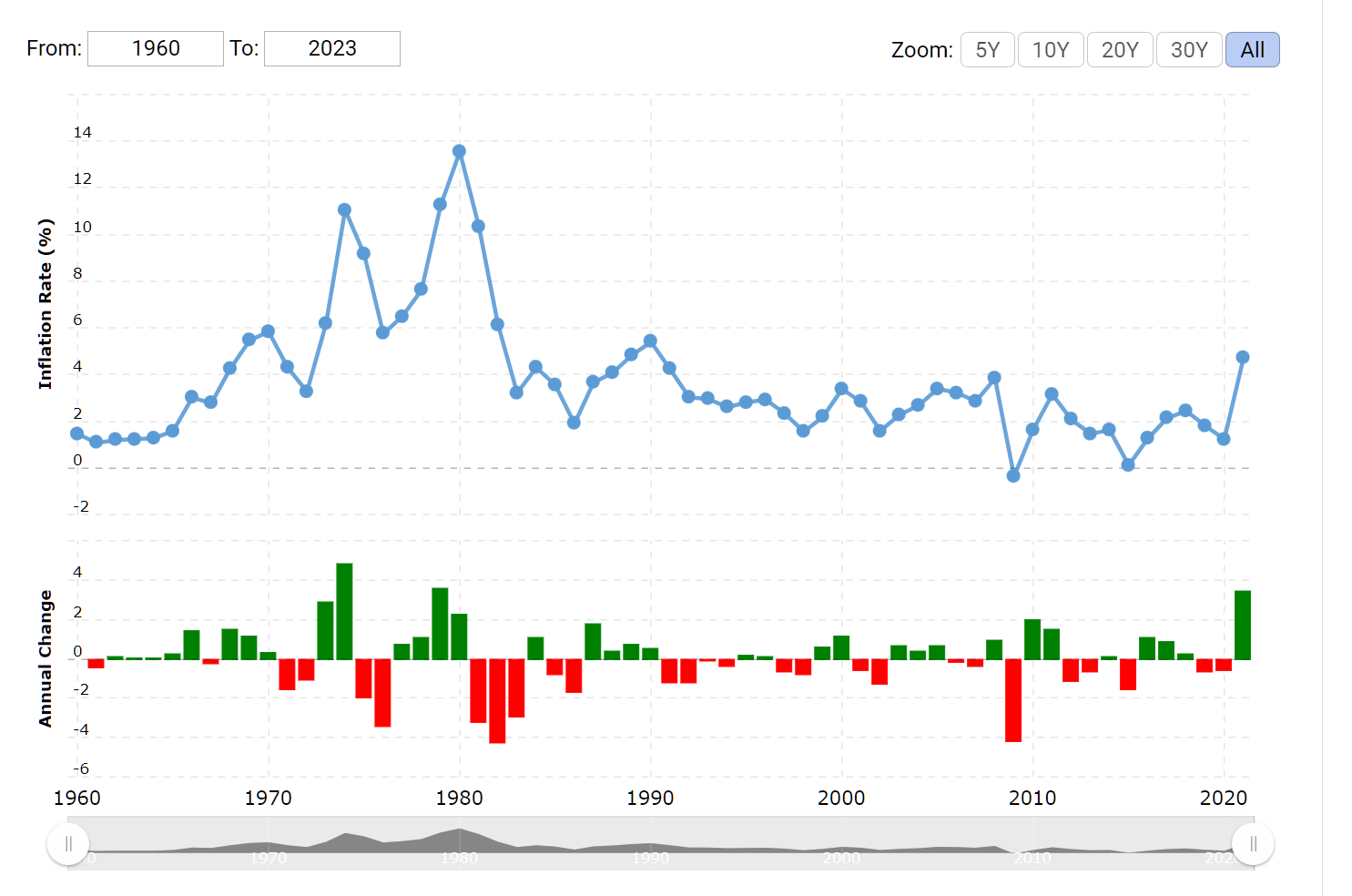
Maybe the take-away should be that Americans today aren’t smarter than Americans were in the 1960s and 1970s. Inflation jumped dramatically in 1966 as Lyndon Johnson and Congress spent like alimony plaintiffs on (1) the Great Society programs of Medicare, Medicaid, etc., and (2) the Vietnam War. The inflation rate did not come down to the pre-1966 level until 1998. Maybe we could argue that inflation was finally whipped by 1992 (chart):
If we’re expecting at least 26 years of elevated inflation, what do we do? For a person who doesn’t already have a house, one reasonable response is for him/her/zir/them to try to get a 100 percent mortgage at today’s 6.5-7 percent 30-year rates. Put some stocks in as collateral as necessary to hit the 100 percent number. If Paul Singer is right that the D.C. technocrats won’t be able to resist inflation-as-usual policies, inflation will render the real cost of borrowing almost $0. If Paul Singer is wrong, there is no prepayment penalty so just refinance if rates fall dramatically.
Full post, including comments