Loyal readers may remember a review here of a book by a Los Angeles Times reporter on America’s taxpayer-fueled heroin habit (see Who funded America’s opiate epidemic? You did.). Empire of Pain: The Secret History of the Sackler Dynasty covers the same story from the angle of the family behind OxyContin. The Sacklers, whose names adorn university and art museum buildings throughout the U.S. and Europe, have been convenient scapegoats, but it turns out that they didn’t do it alone. Some things that I learned from the book…
Arthur M. Sackler, the patriarch, died before OxyContin was invented (the slow-release coating was actually the invention of a British company that had been acquired by the Sacklers’ sleepy Purdue Pharma and was used originally for morphine pills called “MS Contin”). He was the significant art collector and benefactor of AOC’s party venue at the Metropolitan Museum (how did it cost $587 for a car ride from the Bronx to the Upper East Side?). With the help of some friendly bureaucrats at the FDA, who would go on to be of much greater assistance to his brothers’ company Purdue, he pushed the limits of what was legal/ethical in medical advertising, especially for Valium and Librium, but museums are still happy to display the name of Hoffmann-La Roche, which actually made the drugs.
The book describes McKinsey, “The firm that built the house of Enron”, working to help Purdue Pharma increase sales of OxyContin even after the company and three executives had pleaded guilty to federal crimes regarding claims made regarding the drug. McKinsey’s biggest idea, according to the author, was that Purdue Pharma’s salespeople should make more frequent calls on the doctors who were the biggest prescribers, i.e., the “pill mills” such as Eleanor Santiago‘s (1 million pills, which resulted in a 20-month prison sentence for the physician). McKinsey also consulted for Johnson & Johnson, the author says, to help them push more opioids out to consumers. (See “Behind the Scenes, McKinsey Guided Companies at the Center of the Opioid Crisis” (NYT 2022))
Speaking of Johnson & Johnson, they owned a division in Tasmania where all of the poppies were grown to enable the production of OxyContin and competitive opioid pills from Janssen (J&J’s pharma subsidiary, now famous for its never-FDA-approved one-shot COVID vaccine) and other companies (in-depth background). The Federal DEA was also complicit in allowing a massive increase in the import quota for this critical raw material.
The author describes Mary Jo White, later appointed by Barack Obama to chair the Securities and Exchange Commission, as instrumental in weakening the government’s efforts to punish Purdue, which was owned entirely by the Sacklers (not, however, by any of Arthur M’s descendants or cash-hungry former wives, “the Valium Sacklers” as opposed to the “OxyContin Sacklers”).
Consistent with Dreamland, the book previously reviewed here, Empire of Pain says that it was common for people to transition from Oxy to heroin sold by migrants from Nayarit, Mexico and that, in fact, 80 percent of heroin overdoses were among people who’d previously been prescribed OxyContin. (See also “From Nayarit to Your Neighborhood: Heroin’s Path to a Ready Local Market”.)
The book supports the heritability of success theory advanced in The Son Also Rises: economics history with everyday applications. Even after a couple of generations that could have succumbed to idleness, the Sackler descendants are reasonably hard-working and successful. Madeleine Sackler, for example, has been successful as a filmmaker (ironically, a couple of them are about life in prison, which is not unrelated to the drug that has funded her lifestyle).
Empire of Pain: The Secret History of the Sackler Dynasty is timely given that a lot of our American brothers, sisters, and binary-resisters were just paid $600/week to stay home for two years and consume drugs and alcohol (this Senate document says there was a 30 percent increase in overdose deaths, but blames the “pandemic” rather than the “lockdown”). The antiracism experts at Mass General say that heavy drinking increased by 21 percent during lockdown.
If nothing else, reading the book will make you cautious about taking that first bottle of painkillers that a doctor prescribes!
The author is a New Yorker writer and he asserts as fact that HIV/AIDS would have been a solved problem if Republicans had not blocked federal funding for research into a cure for this disease (yet SARS-CoV-2 continues to kill steadily despite literally $trillions in tax money that has been thrown at it; see Did vaccines or any other intervention slow down COVID?). He also asserts as fact that if Purdue Pharma was liable for opioid-related deaths then gun manufacturers are obviously liable for shooting deaths (never mentioning that the gun manufacturers have always been quite candid about the lethality of guns/bullets and that the theory of liability for the opioid industry is that the companies lied to Americans about heroin-style drugs not being addictive/harmful).
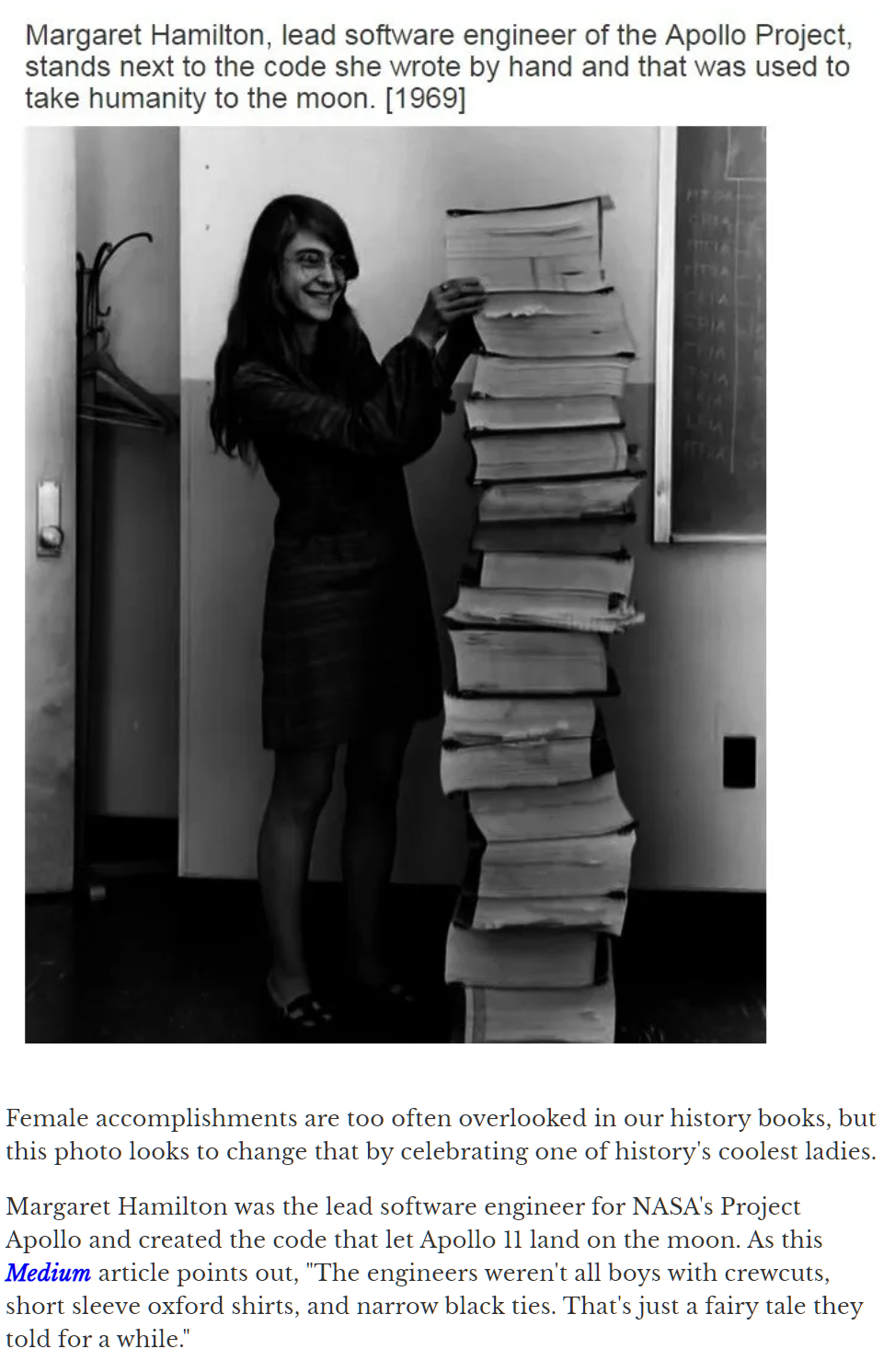
Loosely related… the Temple of Dendur at the Met, in what used to be called “The Sackler Wing” (funded by Arthur M, blameless in the OxyContin debacle), “temporarily closed” in June 2021 for coronapanic:
Full post, including comments