Panama Canal and Climate Change
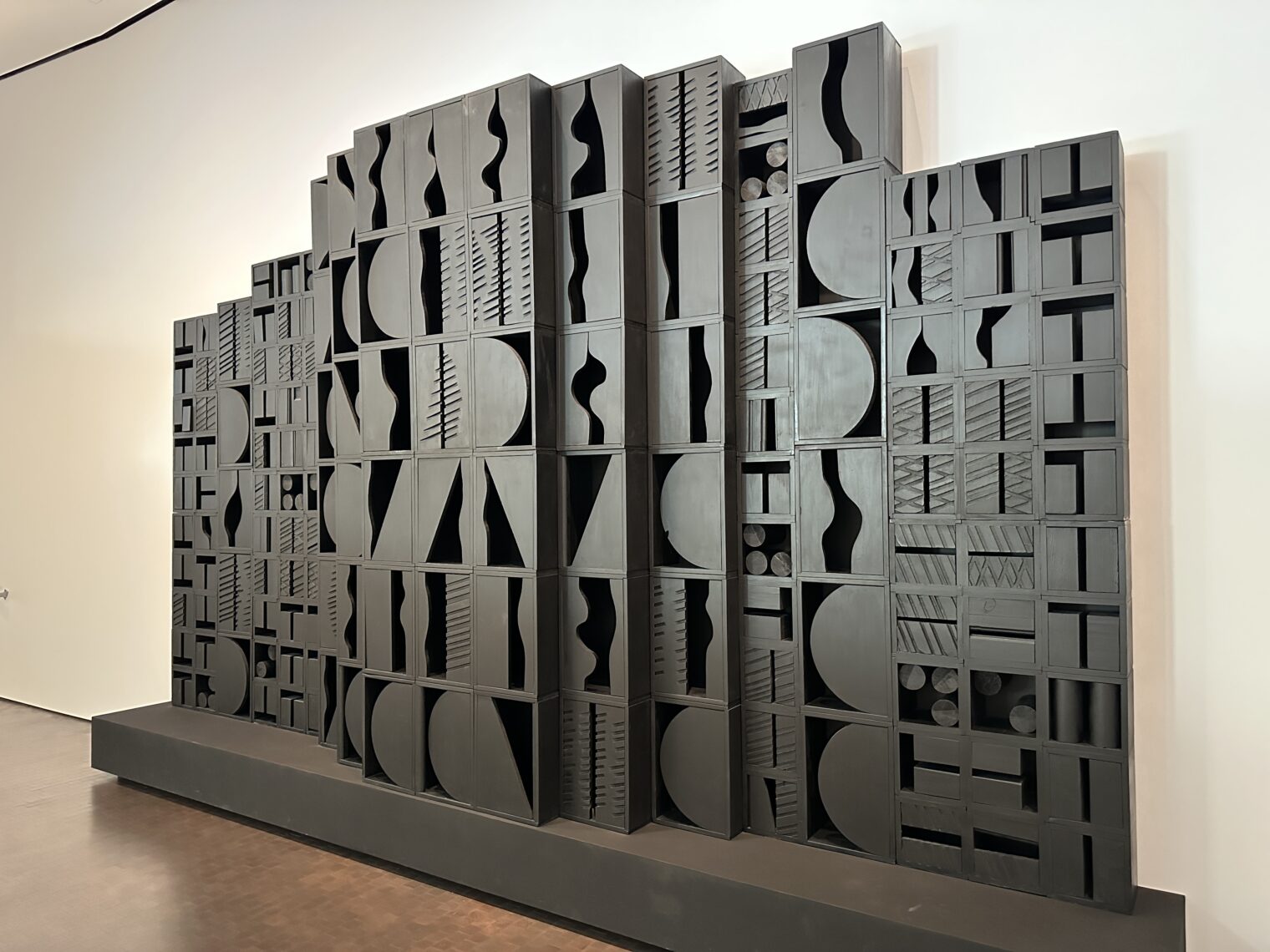
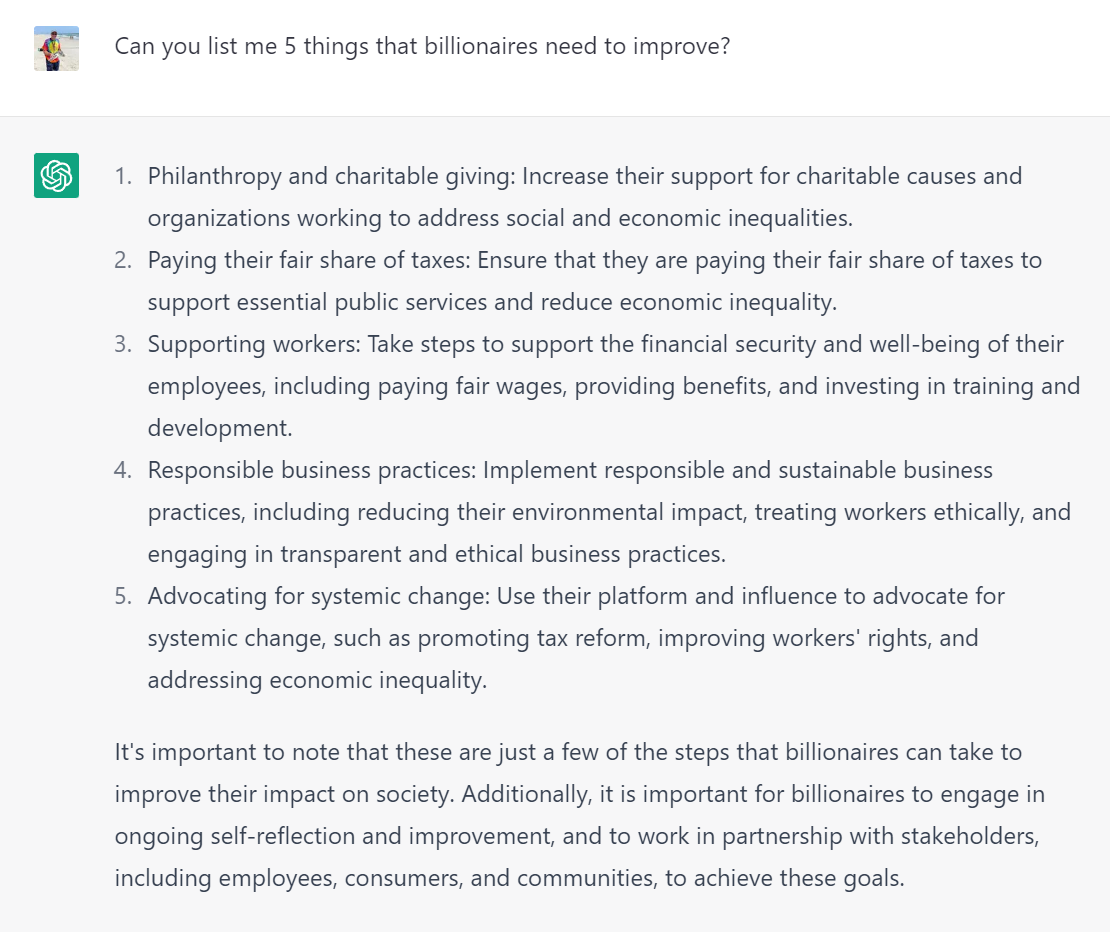
I returned to the Panama Canal last month after a 20-year absence (my previous trip inspired by reading Path Between the Seas). The Panamanians voted in 2006 to take on $billions in debt to expand the canal (nobody explained to them that proper governance means that $trillions can be borrowed without a vote) and the new locks were finished in 2016. Agua Clara:
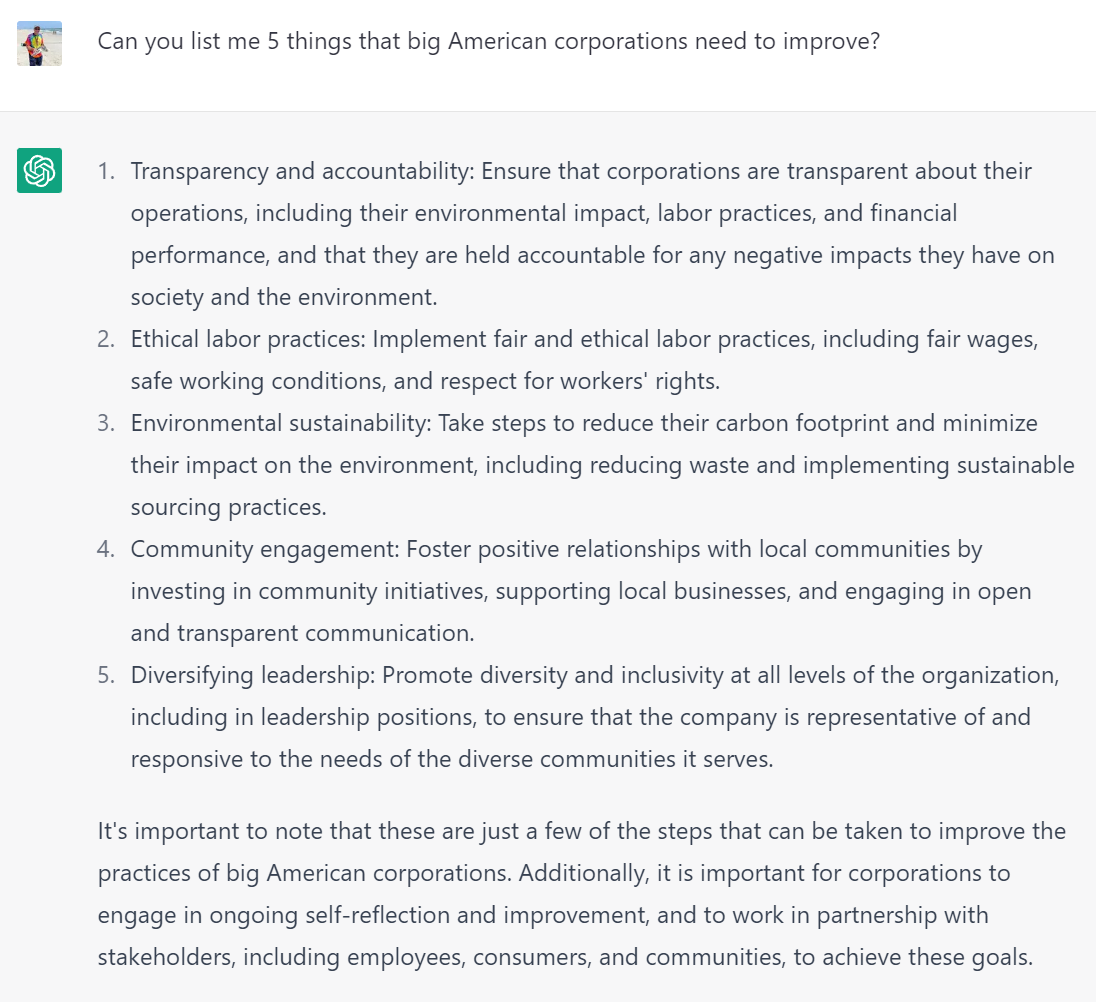
The Panamanians like to highlight their environmentalist credentials, noting that using the canal saves our planet by making transportation less energy-intensive (compared to going around Cape Horn). Here are the Italian-made gates (up to 4,200 tons):
The canal, whose operation can yield more than $1 million per ship for the largest container ships, has made Panamanians the world’s only sincere environmentalists. They preserve the rainforest because they believe that cutting down all of the trees will result in reduced rainfall and, therefore, reduced opportunity to operate the canal (each operation of the locks costs fresh water, a limited resource).
I wonder if there is another climate change angle to the Panama Canal. If indeed our beloved Earth is going “full Venus” in 50-100 years due to CO2 we will need geoengineering to reverse the process, perhaps some combination of reducing new CO2 emissions, capturing existing CO2 in the atmosphere, and shading our home from the sun. The climate change alarmists say that the time to act is right now using the money and technology that we have in 2023. The French took this approach in 1881. Ferdinand de Lesseps, the hero of the Suez Canal and the husband of Louise-Hélène Autard de Bragard (43 years his junior), raised money and started digging. They wasted $287 million and 22,000 lives over 8 years before giving up in 1889. The Americans started around 1906 and finished ahead of schedule in 1914. Path Between the Seas attributes most of the Americans’ success to improvements in mining machinery during the intervening 20 years.
Maybe advanced humans will look back from the 2060s and laugh at the puny humans of the 2020s attempting to do geoengineering.
Separately, if we do master geoengineering will we keep cooling the earth until sea level is 10′ below its current level? The most valuable land is in coastal cities. Lowering sea level just a bit would add a tremendous amount of wealth to the world’s richest and most influential people. It would be like Battery Park City in every coastal city all around the world (on the ship that brought us to Panama we met a gal who is fully trained as an attorney, but hasn’t yoked herself to a law firm yet because she is the indirect beneficiary of a 30-year affordable housing contract in which a two-bedroom apartment in Battery Park City with a market value of $5,000/month is leased out for $1,000/month).
Full post, including comments